Your Baby
How big is my baby?
At the start of week 6 the length of your baby is no greater than 2-4mm (0.08 - 0.16 inches) from the top of it's head to it's rump. The crown-rump measurement, rather than the crown-toe measurement is used because your baby's legs bend up towards the body in utero, making it difficult to get an accurate crown-toe measurement.
How does the embryo develop this week?
Week 6 is a busy one, and marks the start of the embryonic period (weeks 6-10 of your pregnancy). During the embryonic period the basic foundations for your baby's life are set, so the embryo is sensitive to any negative factors (alcohol, nicotine, excess caffeine, chemicals and pollutants) that may hinder it's development.
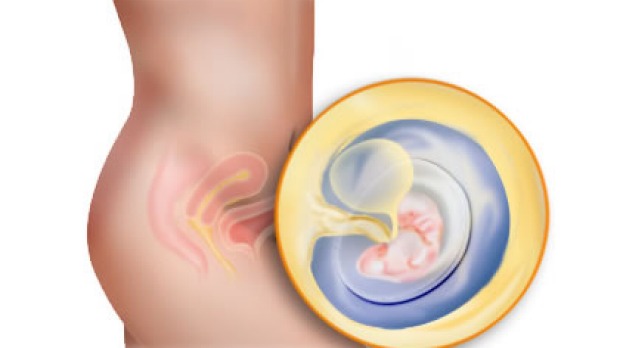
This week the embryo develops 2 cavities, the amniotic sac and the yolk sac. The amniotic sac continues to enlarge and gradually envelops the embryo and body stalk. The yolk sac never attains a large size and disappears as soon as the fetus begins to obtain nourishment from the placenta. The body stalk that connects the embryo to the developing placenta (trophoblast) gradually becomes elongated and develops into the umbilical cord, containing 2 arteries and a single vein.
By week 6 your baby's heart is prominent and beating. The next step is the development of your baby's owns unique blood vessels, and a blood supply that is completely separate to yours. Your baby's circulation first uses the resources of the yolk sac, then later the placenta. Its circulation is closed (covered by the trophoblastic covering) and does not mix directly with your blood. It is your blood that is open to the uterus and feeds the baby, so if placental separation occurs, your blood will be lost, and not the baby's.
By the middle of the week the neural tube closes at your baby's head, where it will form the early brain chambers. By the end of the week the tube has also closed at the bottom of your baby's back. The arm and leg buds are forming and various organs and other body systems are under way.
With all these physical changes, the embryo develops from a layered disc to adopt a C-shaped curvature, taking on a curved body form with a head and tail.
Your Pregnancy
What pregnancy symptoms will I be experiencing?
This week you may start to develop other more noticeable signs of pregnancy, such as nausea possibly accompanied by vomiting (especially in the morning), breast soreness or tenderness, the need to urinate more frequently, fatigue, and constipation. Do not use laxatives without first talking to your doctor. Try to exercise, drink more fluids and eat foods that are high in fibre.
What is an ectopic pregnancy and how is it diagnosed?
An ectopic pregnancy is the result of a blastocyst failing to implant in the uterus, and instead implanting somewhere else - almost always the fallopian tube. Ectopic pregnancy occurs in approximately 1 in every 100 pregnancies, and is more likely to occur when there has been damage to the fallopian tube.
The growing embryo pushes against the fallopian tube, weakening its walls and eventually causing the tube to burst. Before this happens, there are signs that indicate a possible ectopic pregnancy. You will still receive a positive urine test if you have an ectopic pregnancy, so it can be difficult to detect until you experience the warning signs. These will most likely include abdominal pain (usually on one side), possibly accompanied by vaginal bleeding, fainting and nausea. If you experience any of these symptoms they should be reported to your health care professional immediately.
Do I need to have any health checks?
When you visit your local GP to confirm and talk about your pregnancy, he/she will organise routine pregnancy screening blood tests. These are a requirement for all women and the tests check your blood group and Rhesus factor, your iron levels, and whether or not you have any underlying infections or health problems (that can be detected by a blood test).
While you need to take folic acid during pregnancy, you should speak to your doctor before taking any additional vitamin and mineral supplements. Supplements should not be viewed as a substitute for a healthy and nutritious diet.
It is also a good time to start thinking about your "birth choices" and who you would like to be involved in the birth of your baby. There are many options available to you and it is worthwhile exploring the choices to determine what you feel most comfortable with. Pregnancy, birth and early parenthood are very personal and individual experiences. Many health care professionals are happy to discuss the care that they provide without obligation.
The important factor for most mothers-to-be is to remember that pregnancy and birth is essentially a normal, natural and healthy process for women and their families.
What happens when my pregnancy is confirmed?
When your pregnancy is confirmed, you will need to decide where you would like to give birth and who you would like to manage your care during pregnancy and birth. As soon as you have decided how and where you would like to give birth, you can schedule your first appointment with your health care professional.
What happens when I make my first visit to my health care professional?
He/she will obtain a detailed family and medical history. This will highlight any potential areas of concern, such as the risks of continuing to smoke during pregnancy. Other areas that may be covered include diet, exercise, routine tests, alcohol, and any allergies.
A vital piece of information that you provide is the first day of your last menstrual period (LMP). It is this date that determines an expected date of confinement (EDC) or the date you can expect to give birth. If you are unsure of the date of your LMP, a blood test or ultrasound may have to be performed to confirm dates, however a definite LMP is considered to be more accurate.
Some health care professionals advise that a Pap smear be performed at this visit, although research suggests that in the majority of cases, an accurate result cannot be obtained when a woman is pregnant. This is due to changes in the cervix. The more consistent advice is to encourage regular 2nd yearly smears throughout life. Some health care professionals may also perform an internal examination at the first appointment.
What about ultrasound's? When will I have my first ultrasound?
There is no indication that a "routine" ultrasound in the early stages of pregnancy provides any benefit, however if there is an abnormality during this period (such as abdominal pain or vaginal bleeding) it is best to be sure that everything is OK. An ultrasound may also be required early in pregnancy if there is uncertainty about your dates due to long or irregular menstrual cycles.
Your health care professional may not see the need for an ultrasound until 18-19 weeks of pregnancy, however a Nuchal fold / translucency ultrasound screening is usually performed between 11 and 13 weeks and is becoming more routine. This is an ultrasound screening assessment to detect a specific abnormality of the fetus that can be linked to Down's Syndrome. It is a fairly reliable, non-invasive way of assessing the risk of having a baby with Down's syndrome, and carries no risk of miscarriage. The test is conducted by measuring the appearance and amount of fluid that normally accumulates under the skin at the back of your baby's neck. The fluid accumulation tends to increase when the fetus has a chromosomal disorder. The pick-up rate is thought to be 70-80%, depending on your age.
What routine tests will be performed during my pregnancy?
There are a few routine tests that are usually performed throughout your pregnancy. These include:
Urine test - this is usually performed at each ante-natal visit to detect the presence of any infection, detect the presence of sugar which may indicate a lowered tolerance to sugar during pregnancy, detect the presence of protein which may indicate a problem with your kidneys.
Weight - this is usually performed at each antenatal visit to your health care professional to provide a general indication of your weight and weight gain throughout pregnancy. An average weight gain in pregnancy is about 15 kg.
Blood pressure - this is usually performed at each ante-natal visit to provide an average reading so that any changes can be noted, especially late in pregnancy.
How many antenatal appointments will I have during my pregnancy?
On average you will visit or be visited by your health care professional about 12 times. In early pregnancy the visits are spaced further apart, but become more frequent as the birth approaches.
Learn more about your pregnancy
Would you like weekly updates on your pregnancy? Sign up here to receive this information in your inbox.
Read more information on Pregnancy and Birth on Essential Baby.
Discuss Pregnancy in the Essential Baby Forums.