Lymph
| Lymph | |
|---|---|
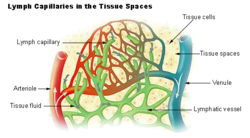
Diagram showing the formation of lymph from interstitial fluid (labeled here as "Tissue fluid"). Note how the tissue fluid is entering the blind ends of lymph capillaries (shown as deep green arrows)
|
|
| Details | |
| Identifiers | |
| Latin | Lympha |
| TA | A12.0.00.043 |
| FMA | 9671 |
| Anatomical terminology | |
Lymph is the fluid that circulates throughout the lymphatic system. The lymph is formed when the interstitial fluid (the fluid which lies in the interstices of all body tissues)[1] is collected through lymph capillaries. It is then transported through larger lymphatic vessels to lymph nodes, where it is cleaned by lymphocytes, before emptying ultimately into the right or the left subclavian vein, where it mixes back with the blood.
Since the lymph is derived from the interstitial fluid, its composition continually changes as the blood and the surrounding cells continually exchange substances with the interstitial fluid. It is generally similar to blood plasma except that it doesn't contain red blood cells. Lymph returns proteins and excess interstitial fluid to the bloodstream. Lymph may pick up bacteria and bring them to lymph nodes, where they are destroyed. Metastatic cancer cells can also be transported via lymph. Lymph also transports fats from the digestive system (beginning in the lacteals) to the blood via chylomicrons.
The word lymph is derived from the name of the ancient Roman deity of fresh water, Lympha.
Contents
Composition[edit]
Lymph has a composition comparable to that of blood plasma, but it may differ slightly. Lymph contains white blood cells. In particular, the lymph that leaves a lymph node is richer in lymphocytes. Likewise, the lymph formed in the human digestive system called chyle is rich in triglycerides (fat), and looks milky white because of its lipid content.
Formation[edit]
Blood supplies nutrients and important metabolites to the cells of a tissue and collects back the waste products they produce, which requires exchange of respective constituents between the blood and tissue cells. This exchange is not direct, but instead is effected through an intermediary called interstitial fluid or tissue fluid, the fluid that occupies the spaces between the cells and constitutes their immediate environment. As the blood and the surrounding cells continually add and remove substances from the interstitial fluid, its composition continually changes. Water and solutes can pass between the interstitial fluid and blood via diffusion across gaps in capillary walls called intercellular clefts; thus, the blood and interstitial fluid are in dynamic equilibrium with each other.[2]
Interstitial fluid forms at the arterial (coming from the heart) end of capillaries because of the higher pressure of blood compared to veins, and most of it returns to its venous ends and venules; the rest (up to 10%) enters the lymph capillaries as lymph.[3] Thus, lymph when formed is a watery clear liquid with the same composition as the interstitial fluid. However, as it flows through the lymph nodes it comes in contact with blood, and tends to accumulate more cells (particularly, lymphocytes) and proteins.[4]
Lymphatic circulation[edit]
Tubular vessels transport lymph back to the blood, ultimately replacing the volume lost during the formation of the interstitial fluid. These channels are the lymphatic channels, or simply lymphatics.[5]
Unlike the cardiovascular system, the lymphatic system is not closed and has no central pump, or lymph hearts (which are found in some animals). Lymph transport, therefore, is slow and sporadic. Despite low pressure, lymph movement occurs due to peristalsis (propulsion of the lymph due to alternate contraction and relaxation of smooth muscle tissue), valves, and compression during contraction of adjacent skeletal muscle and arterial pulsation.[6]
Lymph that enters the lymph vessels from the interstitial spaces usually does not flow backwards along the vessels because of the presence of valves. If excessive hydrostatic pressure develops within the lymph vessels, though, some fluid can leak back into the interstitial spaces and contribute to formation of oedema.
Flow of the lymph in the thoracic duct in an average resting person usually approximates 100ml per hour. Accompanied by another ~25ml per hour in other lymph vessels, total lymph flow in the body is about 4 to 5 liters per day. Which can be elevated several folds in case of exercising. Thus it can be estimated that without lymphatic flow, an average resting person would die within 24 hours. [7]
As a growth medium[edit]
In 1907 the zoologist Ross Granville Harrison demonstrated the growth of frog nerve cell processes in a medium of clotted lymph. It is made up of lymph nodes and vessels.
In 1913, E. Steinhardt, C. Israeli, and R. A. Lambert grew vaccinia virus in fragments of tissue culture from guinea pig corneal grown in lymph.[8]
Notes and references[edit]
- ^ Fluid Physiology: 2.1 Fluid Compartments
- ^ "The Lymphatic System". Human Anatomy (Gray's Anatomy). Retrieved 2012-10-12.
- ^ Warwick, Roger; Peter L. Williams (1973) [1858]. "Angiology (Chapter 6)". Gray's anatomy. illustrated by Richard E. M. Moore (Thirty-fifth ed.). London: Longman. pp. 588–785.
- ^ Sloop, Charles H.; Ladislav Dory; Paul S. Roheim (March 1987). "Interstitial fluid lipoproteins" (PDF). Journal of Lipid Research. 28 (3): 225–237. PMID 3553402. Retrieved 2008-07-07.
- ^ "Definition of lymphatics". Webster's New World Medical Dictionary. MedicineNet.com. Retrieved 2008-07-06.
- ^ Shayan, Ramin; Achen, Marc G.; Stacker, Steven A. (2006). "Lymphatic vessels in cancer metastasis: bridging the gaps". Carcinogenesis. 27 (9): 1729–38. doi:10.1093/carcin/bgl031. PMID 16597644.
- ^ Guyton and Hall Textbook of Medical Physiology. Saunders. 2010. pp. 186, 187. ISBN 978-1416045748.
- ^ Steinhardt, E; Israeli, C; and Lambert, R.A. (1913) "Studies on the cultivation of the virus of vaccinia" J. Inf Dis. 13, 294–300

