Phenoxybenzamine
 |
|
| Clinical data | |
|---|---|
| Trade names | Dibenzyline |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682059 |
| Pregnancy category |
|
| Routes of administration |
Oral |
| ATC code | C04AX02 (WHO) |
| Pharmacokinetic data | |
| Biological half-life | 24 hours |
| Identifiers | |
|
|
| CAS Number | 59-96-1 |
| PubChem (CID) | 4768 |
| IUPHAR/BPS | 7268 |
| DrugBank | DB00925 |
| ChemSpider | 4604 |
| UNII | 0TTZ664R7Z |
| KEGG | D08358 |
| ChEMBL | CHEMBL753 |
| ECHA InfoCard | 100.000.406 |
| Chemical and physical data | |
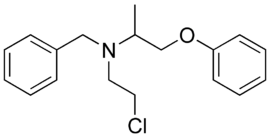
| Formula | C18H22ClNO |
| Molar mass | 303.826 g/mol |
| 3D model (Jmol) | Interactive image |
| Chirality | Racemic mixture |
|
|
|
|
| (verify) | |
Phenoxybenzamine (marketed under the trade name Dibenzyline) is a non-selective, irreversible alpha blocker.
Uses[edit]
It is used in the treatment of hypertension, and specifically that caused by pheochromocytoma. It has a slower onset and a longer-lasting effect compared with other alpha blockers.
It was also the first alpha blocker to be used for treatment of benign prostatic hyperplasia,[1] although it is currently seldom used for that indication due to unfavourable side effects.
It has been used in the treatment of hypoplastic left heart syndrome.[2]
It is also used in complex regional pain syndrome (CPRS) type 1 due to its anti-adrenergic affects. It has shown to be beneficial if used in the first 3 months of the CRPS diagnosis.
Investigational[edit]
Phenoxybenzamine has long been known to block ejaculation without affecting semen quality or ability to achieve orgasm, which could make it an effective male contraceptive. This effect is completely reversible, and is believed to be the result of alpha-1 adrenoceptor blockade in the longitudinal muscles of the vas deferens.[3][4][5] As of 2008, research was underway to identify possible drug candidates that share this effect but act specifically on the reproductive tract, unlike phenoxybenzamine.[3]
Pharmacology[edit]
Phenoxybenzamine is used as an anti-hypertensive due to its efficacy in reducing the vasoconstriction caused by epinephrine (adrenaline) and norepinephrine. Phenoxybenzamine forms a permanent covalent bond with adrenergic receptors. Based on known information about the structures of these receptors, it likely involves attack by the cysteine at position 3.36 in transmembrane helix 3 to form a stable linkage.[6] Thus, it remains permanently bound to the receptor, preventing adrenaline and noradrenaline from binding. This causes vasodilatation in blood vessels, due to its antagonistic effect at the alpha-1 adrenoceptor found in the walls of blood vessels, resulting in a drop in blood pressure. A side effect of phenoxybenzamine is reflex tachycardia.
As a non-selective alpha receptor antagonist, it will also affect both the postsynaptic alpha 1 and presynaptic alpha 2 receptors in the nervous system, and so reduce sympathetic activity. This results in further vasodilation, pupil constriction, an increase in GI tract motility and secretions, and glycogen synthesis.
Clinically, non-selective alpha antagonists block alpha receptors (but do not differentiate between alpha-1 and alpha-2). They are used as antihypertensives because they block alpha-receptor-mediated vasoconstriction. The block on alpha-2 receptors further potentiates beta-effects, increasing cardiac output.
Phenoxybenzamine has a long-lasting action, binding covalently to the alpha receptors. Its only current clinical use is in preparing patients with phaeochromocytoma for surgery; its irreversible antagonism and the resultant depression in the maximum of the agonist dose-response curve are desirable in a situation where surgical manipulation of the tumour may release a large bolus of pressor amine into the circulation. Typically, phenoxybenzamine is not used in the long term, as new receptors are made to upregulate alpha stimulation. The main limiting side-effects of alpha antagonists is that the baroreceptor reflex is disrupted and thus this can cause postural hypotension.
Phenoxybenzamine also has irreversible antagonist/weak partial agonist properties at the serotonin 5-HT2A receptor.[7][8][9][10] Due to its 5-HT2A receptor antagonism, phenoxybenzamine is useful in the treatment of carcinoid tumor, a neoplasm that secretes large amounts of serotonin and causes diarrhea, bronchoconstriction, and flushing.[8]
See also[edit]
References[edit]
- ^ Caine M, Perlberg S, Meretyk S (1978). "A placebo-controlled double-blind study of the effect of phenoxybenzamine in benign prostatic obstruction". British journal of urology. 50 (7): 551–4. doi:10.1111/j.1464-410X.1978.tb06210.x. PMID 88984.
- ^ Guzzetta NA (August 2007). "Phenoxybenzamine in the treatment of hypoplastic left heart syndrome: a core review". Anesth. Analg. 105 (2): 312–5. doi:10.1213/01.ane.0000275185.44796.92. PMID 17646482.
- ^ a b Aitken RJ, Baker MA, Doncel GF, Matzuk MM, Mauck CK, Harper MJ (April 2008). "As the world grows: contraception in the 21st century". J Clin Invest. 118 (4): 1330–43. doi:10.1172/JCI33873. PMC 2276786
 . PMID 18382745.
. PMID 18382745. - ^ Kjaergaard N, Kjaergaard B, Lauritsen JG (June 1988). "Prazosin, an adrenergic blocking agent inadequate as male contraceptive pill". Contraception. 37 (6): 621–9. doi:10.1016/0010-7824(88)90008-X. PMID 2899490.
- ^ Homonnai ZT, Shilon M, Paz GF (May 1984). "Phenoxybenzamine—an effective male contraceptive pill". Contraception. 29 (5): 479–91. doi:10.1016/0010-7824(84)90022-2. PMID 6430643.
- ^ Frang H, Cockcroft V, Karskela T, Scheinin M, Marjamäki A (2001). "Phenoxybenzamine binding reveals the helical orientation of the third transmembrane domain of adrenergic receptors". J. Biol. Chem. 276 (33): 31279–84. doi:10.1074/jbc.M104167200. PMID 11395517.
- ^ Doggrell, S. A. (1995). "Increase in affinity and loss of 5-hydroxytryptamine2A-receptor reserve for 5-hydroxytryptamine on the aorta of spontaneously hypertensive rats". Journal of Autonomic Pharmacology. 15 (5): 371–377. doi:10.1111/j.1474-8673.1995.tb00403.x. ISSN 0144-1795.
- ^ a b Anthony Trevor; Bertram Katzung; Susan Masters (2008). Katzung & Trevor's Pharmacology Examination and Board Review: Eighth Edition. McGraw Hill Professional. pp. 153, 500. ISBN 978-0-07-148869-3.
- ^ B. Olivier; I. van Wijngaarden; W. Soudijn (10 July 1997). Serotonin Receptors and their Ligands. Elsevier. pp. 206–. ISBN 978-0-08-054111-2.
- ^ Timothy S. Gaginella; James J. Galligan (25 July 1995). Serotonin and Gastrointestinal Function. CRC Press. pp. 56–. ISBN 978-0-8493-8387-8.