Vitamin B6
| Vitamin B6 | |
|---|---|
| Drug class | |
|
|
| Class identifiers | |
| Use | Vitamin B6 deficiency |
| ATC code | A11HA02 |
| Biological target | enzyme cofactor |
| Clinical data | |
| Drugs.com | International Drug Names |
| External links | |
| MeSH | D025101 |
| In Wikidata | |
Vitamin B6 refers to a group of chemically very similar compounds which can be interconverted in biological systems. Vitamin B6 is part of the vitamin B group, and its active form, pyridoxal 5′-phosphate (PLP) serves as a coenzyme in many enzyme reactions in amino acid, glucose, and lipid metabolism.
Contents
Forms[edit]
|
|
This article needs more medical references for verification or relies too heavily on primary sources. (October 2016) |
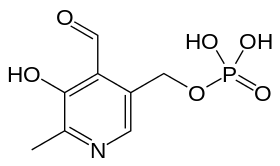
Several forms (vitamers) of vitamin B6 are known:
- Pyridoxine (PN), the form most commonly given as vitamin B6 supplement[citation needed]
- Pyridoxine 5′-phosphate (P5P)
- Pyridoxal (PL)
- Pyridoxal 5′-phosphate (PLP), the metabolically active form (sold as P-5-P vitamin supplement)[citation needed]
- Pyridoxamine (PM)
- Pyridoxamine 5′-phosphate (PMP)
- 4-Pyridoxic acid (PA), the catabolite which is excreted in urine
- Pyritinol, a semi-synthetic derivative of pyridoxine, where two pyridoxine moieties are bound by a disulfide bridge.
All forms except pyridoxic acid[1] and pyritinol can be interconverted. Absorbed pyridoxamine is converted to PMP by pyridoxal kinase, which is further converted to PLP by pyridoxamine-phosphate transaminase or pyridoxine 5′-phosphate oxidase[2] which also catalyzes the conversion of PNP to PLP. Pyridoxine 5′-phosphate oxidase is dependent on flavin mononucleotide (FMN) as a cofactor which is produced from riboflavin (vitamin B2) i.e. in this biochemical pathway, dietary vitamin B6 cannot be used without vitamin B2.
Functions[edit]
PLP, the metabolically active form of vitamin B6, is involved in many aspects of macronutrient metabolism, neurotransmitter synthesis, histamine synthesis, hemoglobin synthesis and function, and gene expression. PLP generally serves as a coenzyme (cofactor) for many reactions including decarboxylation, transamination, racemization, elimination, replacement, and beta-group interconversion.[3] The liver is the site for vitamin B6 metabolism.
Amino acid metabolism[edit]
- PLP is a cofactor in the biosynthesis of five important neurotransmitters: serotonin, dopamine, epinephrine, norepinephrine, and gamma-aminobutyric acid (GABA). PLP is also involved in the synthesis of histamine.
- Transaminases break down amino acids with PLP as a cofactor. The proper activity of these enzymes is crucial for the process of moving amine groups from one amino acid to another.
- Serine racemase which synthesizes the neuromodulator serine is a PLP-dependent enzyme.
- PLP is a coenzyme needed for the proper function of the enzymes cystathionine synthase and cystathionase. These enzymes catalyze reactions in the catabolism of methionine. Part of this pathway (the reaction catalyzed by cystathionase) also produces cysteine.
- Selenomethionine is the primary dietary form of selenium. PLP is needed as a cofactor for the enzymes that allow selenium to be used from the dietary form. PLP also plays a cofactor role in releasing selenium from selenohomocysteine to produce hydrogen selenide, which can then be used to incorporate selenium into selenoproteins.
- PLP is required for the conversion of tryptophan to niacin, so low vitamin B6 status impairs this conversion.[3][4]
Glucose metabolism[edit]
PLP is a required coenzyme of glycogen phosphorylase, the enzyme necessary for glycogenolysis to occur.[3] PLP can catalyze transamination reactions that are essential for providing amino acids as a substrate for gluconeogenesis.
Lipid metabolism[edit]
PLP is an essential component of enzymes that facilitate the biosynthesis of sphingolipids.[3] Particularly, the synthesis of ceramide requires PLP. In this reaction, serine is decarboxylated and combined with palmitoyl-CoA to form sphinganine, which is combined with a fatty acyl-CoA to form dihydroceramide. Dihydroceramide is then further desaturated to form ceramide. In addition, the breakdown of sphingolipids is also dependent on vitamin B6 because sphingosine-1-phosphate lyase, the enzyme responsible for breaking down sphingosine-1-phosphate, is also PLP-dependent.
Hemoglobin synthesis and function[edit]
PLP aids in the synthesis of hemoglobin, by serving as a coenzyme for the enzyme ALA synthase.[5] It also binds to two sites on hemoglobin to enhance the oxygen binding of hemoglobin.[3]
Gene expression[edit]
PLP has been implicated in increasing or decreasing the expression of certain genes. Increased intracellular levels of the vitamin lead to a decrease in the transcription of glucocorticoids. Also, vitamin B6 deficiency leads to the increased gene expression of albumin mRNA. Also, PLP influences expression of glycoprotein IIb by interacting with various transcription factors. The result is inhibition of platelet aggregation.[3]
Nutrition[edit]
Food sources[edit]
Vitamin B6 is widely distributed in foods in both its free and bound forms. Cooking, storage, and processing losses of vitamin B6 vary and in some foods may be more than 50%,[6] depending on the form of vitamin present in the food. Plant foods lose the least during processing, as they contain mostly pyridoxine, which is far more stable than the pyridoxal or pyridoxamine found in animal foods. For example, milk can lose 30–70% of its vitamin B6 content when dried.[3] Vitamin B6 is found in the germ and aleurone layer of grains, and milling results in the reduction of this vitamin in white flour. The heating that occurs before most freezing and canning processes are other methods that may result in the loss of vitamin B6 in foods.[7]
Foods that contain large amounts of vitamin B6 include pork,[8] turkey,[9] beef,[10] bananas,[11] chickpeas,[12] potatoes,[13] and pistachios.[14]
Dietary reference intake[edit]
The Food and Nutrition Board (FNB) of the U.S. Institute of Medicine updated Estimated Average Requirements (EARs) and Recommended Dietary Allowances (RDAs) for vitamin B6 in 1998. The current EARs for vitamin B6 for women and men ages 14 and up increase with age from 1.0 to 1.3 mg/day and from 1.1 to 1.4 mg/day, respectively; the RDAs increase with age from 1.2 to 1.5 and from 1.3 to 1.7 mg/day, respectively. RDAs are higher than EARs so as to identify amounts that will cover people with higher than average requirements. RDA for pregnancy equals 1.9 mg/day. RDA for lactation equals 2.0 mg/day. For infants up to 12 months the Adequate Intake (AI) is 0.1–0.3 mg/day. and for children ages 1–13 years the RDA increases with age from 0.5 to 1.0 mg/day. As for safety, the FNB sets Tolerable Upper Intake Levels (known as ULs) for vitamins and minerals when evidence is sufficient. In the case of vitamin B6 the UL is set at 100 mg/day.[15] The European Food Safety Authority reviewed the same safety question and set its UL at 25 mg/day.[16] Safety issues are presented at length in the Toxicity section. Collectively the EARs, RDAs, AIs and ULs are referred to as Dietary Reference Intakes.
For U.S. food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of daily value (%DV). For vitamin B6 labeling purposes 100% of the Daily Value was 2.0 mg, but as of May 2016 it has been revised to 1.7 mg. A table of the pre-change adult Daily Values is provided at Reference Daily Intake. Food and supplement companies have until July 28, 2018 to comply with the change.
Absorption and excretion[edit]
Vitamin B6 is absorbed in the jejunum and ileum by passive diffusion. With the capacity for absorption being so great, animals are able to absorb quantities much greater than necessary for physiological demands. The absorption of pyridoxal phosphate and pyridoxamine phosphate involves their dephosphorylation catalyzed by a membrane-bound alkaline phosphatase. Those products and nonphosphorylated forms in the digestive tract are absorbed by diffusion, which is driven by trapping of the vitamin as 5′-phosphates through the action of phosphorylation (by a pyridoxal kinase) in the jejunal mucosa. The trapped pyridoxine and pyridoxamine are oxidized to pyridoxal phosphate in the tissue.[3]
The products of vitamin B6 metabolism are excreted in the urine, the major product of which is 4-pyridoxic acid. An estimated 40–60% of ingested vitamin B6 is oxidized to 4-pyridoxic acid. Several studies have shown that 4-pyridoxic acid is undetectable in the urine of vitamin B6-deficient subjects, making it a useful clinical marker to assess the vitamin B6 status of an individual.[3] Other products of vitamin B6 metabolism excreted in the urine when high doses of the vitamin have been given include pyridoxal, pyridoxamine, and pyridoxine and their phosphates. A small amount of vitamin B6 is also excreted in the feces.
Deficiency[edit]
Signs and symptoms[edit]
The classic clinical syndrome for vitamin B6 deficiency is a seborrhoeic dermatitis-like eruption, atrophic glossitis with ulceration, angular cheilitis, conjunctivitis, intertrigo, and neurologic symptoms of somnolence, confusion, and neuropathy[17] (due to impaired sphingosine synthesis) and sideroblastic anemia (due to impaired heme synthesis).
Less severe cases present with metabolic lesions[clarify] associated with insufficient activities of the coenzyme PLP. The most prominent of the lesions is due to impaired tryptophan–niacin conversion. This can be detected based on urinary excretion of xanthurenic acid after an oral tryptophan load. Vitamin B6 deficiency can also result in impaired transsulfuration of methionine to cysteine. The PLP-dependent transaminases and glycogen phosphorylase provide the vitamin with its role in gluconeogenesis, so deprivation of vitamin B6 results in impaired glucose tolerance.[3]
Diagnosis[edit]
The assessment of vitamin B6 status is essential, as the clinical signs and symptoms in less severe cases are not specific.[18] The three biochemical tests most widely used are the activation coefficient for the erythrocyte enzyme aspartate aminotransferase, plasma PLP concentrations, and the urinary excretion of vitamin B6 degradation products, specifically urinary PA. Of these, plasma PLP is probably the best single measure, because it reflects tissue stores.[19] Plasma PLP less than 10 nmol/l is indicative of vitamin B6 deficiency.[19] A PLP concentration greater than 20 nmol/l has been chosen as a level of adequacy for establishing Estimated Average Requirements and Recommended Daily Allowances in the USA.[15] Urinary PA is also an indicator of vitamin B6 deficiency; levels of less than 3.0 mmol/day is suggestive of vitamin B6 deficiency.[20]
Also liver test AST ALT can be low due to pyridoxine deficiency
The classic syndrome for vitamin B6 deficiency is rare, even in developing countries. A handful of cases were seen between 1952 and 1953, particularly in the United States, and occurred in a small percentage of infants who were fed a formula lacking in pyridoxine.[21]
Causes[edit]
A deficiency of vitamin B6 alone is relatively uncommon and often occurs in association with other vitamins of the B complex. The elderly and alcoholics have an increased risk of vitamin B6 deficiency, as well as other micronutrient deficiencies.[22] Evidence exists for decreased levels of vitamin B6 in women with type 1 diabetes and in patients with systemic inflammation, liver disease, rheumatoid arthritis, and those infected with HIV.[23][24][25] Use of oral contraceptives and treatment with certain anticonvulsants, isoniazid, cycloserine, penicillamine, and hydrocortisone negatively impact vitamin B6 status.[26][27][28] Hemodialysis reduces vitamin B6 plasma levels.[29]
There are indications that B6 deficiency can be influenced by theophylline in medication or malnutrition.[medical citation needed]
Treatment[edit]
Treatment of vitamin B6 deficiency lies with replacement, usually in the form of pyridoxine hydrochloride, orally, as a nasal spray, or for injection when in its solution form.
Side effects[edit]
Adverse effects have been documented from vitamin B6 supplements, but never from food sources. Toxicologic animal studies identify specific destruction of the dorsal root ganglia[30] which is documented in human cases of overdose of pyridoxine.[31] Although it is a water-soluble vitamin and is excreted in the urine, doses of pyridoxine in excess of the RDI over long periods of time result in painful and ultimately irreversible neurological problems.
The primary symptoms are pain and numbness of the extremities. In severe cases, motor neuropathy may occur with "slowing of motor conduction velocities, prolonged F wave latencies, and prolonged sensory latencies in both lower extremities", causing difficulty in walking.[32] Sensory neuropathy typically develops at doses of pyridoxine in excess of 1,000 mg per day, but adverse effects can occur with much less, so doses over 200 mg are not considered safe.[33] Symptoms among women taking lower doses have been reported.[34] Two reported cases of neuropathy with pyridoxine treatment of 24 and 40 mg/day may have been coincidental.[33]
Existing authorizations and valuations vary considerably worldwide. In 1993, the European Community Scientific Committee on Food defined intakes of 50 mg of vitamin B6 per day as harmful and established a tolerable upper intake level of 25 mg/day for adults in 2000. The Expert Group on Vitamins and Minerals of the Food Standard Agency UK (UK EVM) derived a safe upper level (SUL) of 10 mg/day for a 60 kg adult in 2003. The tolerable upper limit has been set by the US FDA at 100 mg/day in 2000.[35]
The nutrient reference values in Australia and New Zealand recommend an upper limit of 50 mg a day in adults. "The same figure was set for pregnancy and lactation as there is no evidence of teratogenicity at this level. The UL was set based on metabolic body size and growth considerations for all other ages and life stages except infancy. It was not possible to set a UL for infants, so intake is recommended in the form of food, milk or formula." "The ULs were set using results of studies involving long-term oral administration of pyridoxine at doses of less than 1 g/day.[15][34][36][37][38][39] A no-observed-adverse-effect level (NOAEL) of 200 mg/day was identified from the studies of Bernstein & Lobitz (1988) and Del Tredici et al (1985). These studies involved subjects who had generally been on the supplements for five to six months or less. The study of Dalton and Dalton (1987), however, suggested the symptoms might take substantially longer than this to appear. In this latter retrospective survey, subjects who reported symptoms had been on supplements for 2.9 years, on average. Those reporting no symptoms had taken supplements for 1.9 years."[40]
Because no placebo-controlled studies show therapeutic benefits of high doses of pyridoxine, and the well-documented occurrence of significant toxic effects, little reason exists to exceed the RDI using supplements unless under medical supervision (e.g. in treatment of primary hyperoxaluria).
History[edit]
In 1934, the Hungarian physician Paul György discovered a substance that was able to cure a skin disease in rats (dermititis acrodynia). He named this substance vitamin B6.[41][42] In 1938, Samuel Lepkovsky isolated vitamin B6 from rice bran. Harris and Folkers in 1939 determined the structure of pyridoxine, and, in 1945, Snell was able to show the two forms of vitamin B6, pyridoxal and pyridoxamine. Vitamin B6 was named pyridoxine to indicate its structural homology to pyridine.
See also[edit]
References[edit]
| This article lacks ISBNs for the books listed in it. (July 2016) |
- ^ Johannson, S.; Lindstedt, S.; Tiselius, H. (1973). "Metabolic interconversions of different forms of Vitamin B6" (PDF). J. Biol. Chem. 249 (19): 6040–6046. PMID 4418204.
- ^ Ink, S. L.; Henderson, L. M. (1984). "Vitamin B6 metabolism". Annu. Rev. Nutr. 4 (1): 455–470. doi:10.1146/annurev.nu.04.070184.002323. PMID 6380540.
- ^ a b c d e f g h i j Combs, G. F. (2008). The Vitamins: Fundamental Aspects in Nutrition and Health. San Diego: Elsevier.
- ^ Lichtstein, H. C.; Gunsalus, I. C.; Umbreit, W. W. (1945). "Function of the vitamin B6 group; pyridoxal phosphate (codecarboxylase) in transamination" (PDF). J. Biol. Chem. 161 (1): 311–320. PMID 21005738.
- ^ "Heme Synthesis". RPI.edu. doi:10.1042/BJ20030513. Retrieved 2012-11-02.
- ^ McCormick, D. B. (2006). "Vitamin B6". In Bowman, B. A.; Russell, R. M. Present Knowledge in Nutrition. 2 (9th ed.). Washington, DC: International Life Sciences Institute. p. 270.
- ^ Sauberlich, H. (1987). "Vitamins – how much is for keeps?". Nutr. Today. 22: 20–28.
- ^ "10973, Pork, ground, 96% lean / 4% fat, raw". National Nutrient Database for Standard Reference, Release 27. United States Department of Agriculture, Agricultural Research Service. Retrieved 27 June 2015.
- ^ "05305, Ground turkey, raw". National Nutrient Database for Standard Reference, Release 27. United States Department of Agriculture, Agricultural Research Service. Retrieved 27 June 2015.
- ^ "23040, Beef, chuck, shoulder clod, shoulder top and center steaks, separable lean and fat, trimmed to 0" fat, select, cooked, grilled". National Nutrient Database for Standard Reference, Release 27. United States Department of Agriculture, Agricultural Research Service. Retrieved 27 June 2015.
- ^ "09040, Bananas, raw". National Nutrient Database for Standard Reference, Release 27. United States Department of Agriculture, Agricultural Research Service. Retrieved 27 June 2015.
- ^ "16360, Chickpeas (garbanzo beans, bengal gram), mature seeds, canned, solids and liquids, low sodium". National Nutrient Database for Standard Reference, Release 27. United States Department of Agriculture, Agricultural Research Service. Retrieved 27 June 2015.
- ^ "11356, Potatoes, Russet, flesh and skin, baked". National Nutrient Database for Standard Reference, Release 27. United States Department of Agriculture, Agricultural Research Service. Retrieved 27 June 2015.
- ^ "12151, Nuts, pistachio nuts, raw". National Nutrient Database for Standard Reference, Release 27. United States Department of Agriculture, Agricultural Research Service. Retrieved 27 June 2015.
- ^ a b c Food and Nutrition Board Institute of Medicine (1998). Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press.
- ^ Tolerable Upper Intake Levels For Vitamins And Minerals (PDF), European Food Safety Authority, 2006
- ^ Andrews' Diseases of the Skin (10th ed.). Elsevier.
- ^ Gibson, R. S. (2005). "Assessment of vitamin B6 status". Principles of Nutritional Assessment (2nd ed.). New York: Oxford University Press. pp. 575–594.
- ^ a b Liu, A.; Lumeng, L.; Aronoff, G.; Li, T-K. (1985). "Relationship between body store of vitamin B6 and plasma pyridoxal-P clearance: metabolic balance studies in humans". J. Lab. Clin. Med. 106 (5): 491–497. PMID 4056565.
- ^ Leklem, J. (1990). "Vitamin B6: A status report". J. Nutr. 120: 1503–1507. PMID 2243296.
- ^ Menkes, John H. (1980). Textbook of Child Neurology. Henry Kimpton Publishers. ISBN 0-8121-0661-X.
- ^ Bowman, B. A.; Russell, R. M. (2006). Present Knowledge in Nutrition (9th ed.). Washington, DC: ILSI Press. p. 273.
- ^ Massé, P. G.; Boudreau, J.; Tranchant, C. C.; Ouellette, R.; Ericson, K. L. (2012). "Type 1 diabetes impairs vitamin B6 metabolism at an early stage of women's adulthood". Applied Physiology, Nutrition, and Metabolism. 37 (1): 167–175. doi:10.1139/h11-146. PMID 22288928.
- ^ Ulvik, A; Midttun, O.; Pedersen, E. R.; Eussen, S. J.; Nygård, O.; Ueland, P. M. (2014). "Evidence for increased catabolism of vitamin B6 during systemic inflammation". Am. J. Clin. Nutr. 100 (1): 250–255. doi:10.3945/ajcn.114.083196. PMID 24808485.
- ^ Rall, L. C.; Meydani, S. N. (1993). "Vitamin B6 and immune competence". Nutr. Rev. 51 (8): 217–225. doi:10.1111/j.1753-4887.1993.tb03109.x. PMID 8302491.
- ^ Bhagavan, H. N. (1985). "Interaction between vitamin B6 and drugs". In Reynolds, R. D.; Leklem, J. E. Vitamin B6: Its Role in Health and Disease. New York: Liss. pp. 401–415.
- ^ Wilson, S. M.; Bivins, B. N.; Russell, K. A.; Bailey, L. B. (2014). "Oral contraceptive use: impact on folate, vitamin B6, and vitamin B12 status". Nutr. Rev. 69 (10): 572–583. doi:10.1111/j.1753-4887.2011.00419.x. PMID 21967158.
- ^ Schwaninger, M.; Ringleb, P.; Winter, R.; Kohl, B.; Fiehn, W.; Rieser, P. A.; Walter-Sack, I. (1999). "Elevated plasma concentrations of homocysteine in antiepileptic drug treatment". Epilepsia. 40 (3): 345–350. doi:10.1111/j.1528-1157.1999.tb00716.x. PMID 10080517.
- ^ Corken, M.; Porter, J. (2011). "Is vitamin B6 deficiency an under-recognized risk in patients receiving hemodialysis? A systematic review: 2000–2010". Nephrology (Carlton). 16 (7): 619–625. doi:10.1111/j.1440-1797.2011.01479.x. PMID 21609363.
- ^ Perry, T. A.; Weerasuriya, A.; Mouton, P. R.; Holloway, H. W.; Greig, N. H. (2004). "Pyridoxine-induced toxicity in rats: a stereological quantification of the sensory neuropathy". Exp. Neurol. 190 (1): 133–144. doi:10.1016/j.expneurol.2004.07.013. PMID 15473987.
- ^ Schaumburg, H.; Kaplan, J.; Windebank, A.; Vick, N.; Rasmus, S.; Pleasure, D.; Brown, M. J. (1983). "Sensory neuropathy from pyridoxine abuse. A new megavitamin syndrome". N. Engl. J. Med. 309 (8): 445–448. doi:10.1056/nejm198308253090801. PMID 6308447.
- ^ Foca, F. J. (September 1985). "Motor and sensory neuropathy secondary to excessive pyridoxine ingestion". Arch. Phys. Med. Rehabil. 66 (9): 634–636. PMID 2994596.
- ^ a b Katan, M. B. (Nov 12, 2005). "How much vitamin B6 is toxic?". Ned. Tijdschr. Geneeskd. 149 (46): 2545–2546. PMID 16320662.
- ^ a b Dalton, K.; Dalton, M. J. T. (Jul 1987). "Characteristics of pyridoxine overdose neuropathy syndrome". Act. Neurol. Scand. 76 (1): 8–11. doi:10.1111/j.1600-0404.1987.tb03536.x. PMID 3630649.
- ^ Scientific Panel on Food Additives, Flavourings, Processing Aids and Materials in Contact with Food (2008). "Opinion on Pyridoxal 5′-phosphate as a source for vitamin B6 added for nutritional purposes in food supplements" (PDF). The EFSA Journal. 760: 1–13.
- ^ Berger, A.; Schaumburg, H. H. (1984). "More on neuropathy from pyridoxine abuse". N. Engl. J. Med. 311 (15): 986–987. doi:10.1056/nejm198410113111513. PMID 6472428.
- ^ Dalton, K. (1985). "Pyridoxine overdose in premenstrual syndrome". Lancet. 1 (8438): 1168–1169. doi:10.1016/s0140-6736(85)92480-8. PMID 2860378.
- ^ Del Tredici, A. M.; Bernstein, A. L.; Chinn, K. (1985). "Carpal tunnel syndrome and vitamin B6 therapy.". In Reynolds, R. D.; Leklem, J. E. Vitamin B6: Its Role in Health and Disease. New York: Liss. pp. 459–462.
- ^ Parry, G. J.; Bredesen, D. E. (1985). "Sensory neuropathy with low-dose pyridoxine". Neurology. 35 (10): 1466–1468. doi:10.1212/wnl.35.10.1466. PMID 2993949.
- ^ "NHMRC Nutrient Reference Values – Nutrients vitamin B6".
- ^ György, Paul (1934). "Vitamin B2 and the pellagra-like dermatitis in rats". Nature. 133 (3361): 498–499. Bibcode:1934Natur.133..498G. doi:10.1038/133498a0.
- ^ György, P.; Eckardt, R. E. (Sep 1940). "Further investigations on vitamin B6 and related factors of the vitamin B2 complex in rats. Parts I and II". Biochem. J. 34 (8–9): 1143–1154. doi:10.1042/bj0341143. PMC 1265394
 . PMID 16747297.
. PMID 16747297.
External links[edit]
- Facts about Vitamin B6 from Office of Dietary Supplements at National Institutes of Health
- The B6 database A database of B6-dependent enzymes at University of Parma
- COT statement on vitamin B6 (pyridoxine) toxicity (June 1997) (Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment (COT))
- Vitamin B6 at the US National Library of Medicine Medical Subject Headings (MeSH)

