Atenolol
 |
|
 |
|
| Clinical data | |
|---|---|
| Trade names | Tenormin |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a684031 |
| License data | |
| Pregnancy category |
|
| Routes of administration |
Oral or IV |
| ATC code | C07AB03 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 40–50% |
| Protein binding | 6–16% |
| Metabolism | Hepatic <10% |
| Biological half-life | 6–7 hours |
| Excretion | Renal Lactic (In lactiferous females) |
| Identifiers | |
|
|
| CAS Number | 29122-68-7 |
| PubChem (CID) | 2249 |
| IUPHAR/BPS | 548 |
| DrugBank | DB00335 |
| ChemSpider | 2162 |
| UNII | 50VV3VW0TI |
| KEGG | D00235 |
| ChEBI | CHEBI:2904 |
| ChEMBL | CHEMBL24 |
| ECHA InfoCard | 100.044.941 |
| Chemical and physical data | |
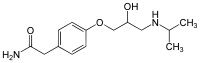
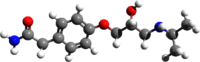
| Formula | C14H22N2O3 |
| Molar mass | 266.336 g/mol |
| 3D model (Jmol) | Interactive image |
| Chirality | Racemic mixture |
|
|
|
|
| (verify) | |
Atenolol is a selective β1 receptor antagonist, a drug belonging to the group of beta blockers (sometimes written β-blockers), a class of drugs used primarily in cardiovascular diseases. Introduced in 1976, atenolol was developed as a replacement for propranolol in the treatment of hypertension. It works by slowing down the heart and reducing its workload. Unlike propranolol, atenolol does not readily pass through the blood–brain barrier, thus decreasing the incidence of central nervous system side effects.[1]
Atenolol is one of the most widely used β-blockers in the United Kingdom and was once the first-line treatment for hypertension.[citation needed] However, recent studies indicate that atenolol may not reduce morbidity or mortality when used to treat hypertension, and may even increase mortality in some subgroups.[2] In addition, the role for β-blockers in general in hypertension was downgraded in June 2006 in the United Kingdom, and later in the United States, as they are less appropriate than newer drugs,[which?] particularly in the elderly.[citation needed]
Medical uses[edit]
Atenolol is used for a number of conditions including hypertension, angina, long QT syndrome, acute myocardial infarction, supraventricular tachycardia, ventricular tachycardia, and the symptoms of alcohol withdrawal.[3]
Off-label uses of atenolol, as with other cardioselective β-blockers, include symptomatic treatment of psychological issues such as anxiety. β-blockers are effective for some in treating the somatic (physical) effects of anxiety. In these instances, dosing is used as needed instead of regular daily dosing.
Due to its hydrophilic (water-attracting) properties, the drug is less suitable in migraine prophylaxis compared to propranolol, because, for this indication, atenolol would have to reach the brain in high concentrations, which is not the case, because atenolol does not pass through the blood–brain barrier.[1]
Side effects[edit]
Atenolol was the main β-blocker identified as carrying a higher risk of provoking type 2 diabetes, leading to its downgrading in the United Kingdom in June 2006 to fourth-line agent in the management of hypertension.[4]
Antihypertensive therapy with atenolol provides weaker protective action against cardiovascular complications (e.g. myocardial infarction and stroke) compared to other antihypertensive drugs. In some cases, diuretics are superior.[5] In addition, atenolol has been found to lack mortality benefits[6][7] and even to increase mortality in older adults.[2]
Overdose[edit]
Symptoms of overdose are due to excessive pharmacodynamic actions on β1 and also β2-receptors. These include bradycardia (slow heartbeat), severe hypotension with shock, acute heart failure, hypoglycemia and bronchospastic reactions. Treatment is largely symptomatic. Hospitalization and intensive monitoring is indicated. Activated charcoal is useful to absorb the drug. Atropine will counteract bradycardia, glucagon helps with hypoglycemia, dobutamine can be given against hypotension and the inhalation of a β2-mimetic as hexoprenalin or salbutamol will terminate bronchospasms. Blood or plasma atenolol concentrations may be measured to confirm a diagnosis of poisoning in hospitalized patients or to assist in a medicolegal death investigation. Plasma levels are usually less than 3 mg/L during therapeutic administration, but can range from 3–30 mg/L in overdose victims.[8][9]
References[edit]
- ^ a b Agon P, Goethals P, Van Haver D, Kaufman JM (August 1991). "Permeability of the blood–brain barrier for atenolol studied by positron emission tomography". Journal of Pharmacy and Pharmacology. 43 (8): 597–600. doi:10.1111/j.2042-7158.1991.tb03545.x. PMID 1681079.
- ^ a b Testa G, Cacciatore F, Della-Morte D, Mazzella F, Mastrobuoni C, Galizia G, Gargiulo G, Rengo F, Bonaduce D, Abete P (2014). "Atenolol use is associated with long-term mortality in community-dwelling older adults with hypertension". Geriatrics & Gerontology International. 14: 153–8. doi:10.1111/ggi.12073. PMID 23581644.
- ^ "Atenolol". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- ^ Sheetal Ladva (28 June 2006). "NICE and BHS launch updated hypertension guideline". National Institute for Health and Clinical Excellence. Archived from the original on 17 June 2008.
- ^ Carlberg B, Samuelsson O, Lindholm LH (2004). "Atenolol in hypertension: is it a wise choice?". The Lancet. 364 (9446): 1684–9. doi:10.1016/S0140-6736(04)17355-8. PMID 15530629.
- ^ Tomiyama H, Yamashina A (2014). "Beta-Blockers in the Management of Hypertension and/or Chronic Kidney Disease". International Journal of Hypertension. 2014: 919256. doi:10.1155/2014/919256. PMC 3941231
 . PMID 24672712.
. PMID 24672712. - ^ DiNicolantonio JJ, Fares H, Niazi AK, Chatterjee S, D'Ascenzo F, Cerrato E, Biondi-Zoccai G, Lavie CJ, Bell DS, O'Keefe JH (2015). "β-Blockers in hypertension, diabetes, heart failure and acute myocardial infarction: a review of the literature". Open Heart. 2: e000230. doi:10.1136/openhrt-2014-000230. PMC 4371808
 . PMID 25821584.
. PMID 25821584. - ^ DeLima LG, Kharasch ED, Butler S (1995). "Successful pharmacologic treatment of massive atenolol overdose: sequential hemodynamics and plasma atenolol concentrations". Anesthesiology. 83 (1): 204–207. doi:10.1097/00000542-199507000-00025. PMID 7605000.
- ^ R. Baselt (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, Calif.: Biomedical Publications. pp. 116–117.
External links[edit]
- Hope, Jenny (6 September 2006). "Beta-blockers 'increase diabetes risk by 50 per cent'". Daily Mail. London.