Rifampicin
 |
|
 |
|
| Clinical data | |
|---|---|
| Pronunciation | /rɪˈfæmpəsɪn/ |
| Trade names | Rifadin, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682403 |
| License data | |
| Pregnancy category |
|
| Routes of administration |
by mouth, IV |
| ATC code | J04AB02 (WHO) QJ54AB02 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 90 to 95% (by mouth) |
| Protein binding | 80% |
| Metabolism | Liver and intestinal wall |
| Biological half-life | 3–4 hours |
| Excretion | Urine (~30%), faeces (60–65%) |
| Identifiers | |
|
|
| CAS Number | 13292-46-1 |
| PubChem (CID) | 5381226 |
| IUPHAR/BPS | 2765 |
| DrugBank | DB01045 |
| ChemSpider | 10468813 |
| UNII | VJT6J7R4TR |
| KEGG | D00211 |
| ChEBI | CHEBI:28077 |
| ChEMBL | CHEMBL374478 |
| NIAID ChemDB | 007228 |
| PDB ligand ID | RFP (PDBe, RCSB PDB) |
| ECHA InfoCard | 100.032.997 |
| Chemical and physical data | |
| Formula | C43H58N4O12 |
| Molar mass | 822.94 g/mol |
| 3D model (Jmol) | Interactive image |
| Melting point | 183 to 188 °C (361 to 370 °F) |
| Boiling point | 1,004.42 °C (1,839.96 °F) [1] |
|
|
|
|
| |
|
Rifampicin, also known as rifampin, is an antibiotic used to treat several types of bacterial infections.[2] This includes tuberculosis, leprosy, and Legionnaire's disease. It is almost always used along with other antibiotics, except when given to prevent Haemophilus influenzae type b and meningococcal disease in people who have been exposed to those bacteria. Before treating a person for a long period of time, measurements of liver enzymes and blood counts are recommended. Rifampicin may be given either by mouth or intravenously.[2]
Common side effects include nausea, vomiting, diarrhea, and loss of appetite. It often turns urine, sweat, and tears a red or orange color. Liver problems or allergic reactions may occur. It is part of the recommended treatment of active tuberculosis during pregnancy, even though its safety in pregnancy is not known. Rifampicin is of the rifamycin group of antibiotics. It works by stopping the production of RNA by bacteria.[2]
Rifampicin was discovered in 1965, marketed in Italy in 1968, and approved in the United States in 1971.[3][4][5] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[6] It is available as a generic medication.[2] The wholesale cost in the developing world is about 3.90 USD a month.[7] In the United States it is expensive, with a month of treatment being about 120 USD.[2][8] Rifampicin is made by the soil bacterium Amycolatopsis rifamycinica.[5]
Contents
Medical uses[edit]
Mycobacteria[edit]
Rifampicin is used for the treatment of tuberculosis in combination with other antibiotics, such as pyrazinamide, isoniazid, and ethambutol.[9] For the treatment of tuberculosis, it is administered daily for at least 6 months.[10] Combination therapy is utilized both to prevent the development of resistance and to shorten the length of treatment.[11] Resistance of Mycobacterium tuberculosis to rifampicin develops quickly when it is used without another antibiotic, with laboratory estimates of resistance rates from 10−7 to 10−10 per tuberculosis bacteria per generation.[12][13]
Rifampicin can be used alone in patients with latent tuberculosis infections to prevent or prolong the development of active disease because only small numbers of bacteria are present. A Cochrane review found no difference in efficacy between a three to four month regimen of rifampicin and a six-month regimen of isoniazid for preventing active tuberculosis in patients not infected with HIV, and patients who received rifampicin had a lower rate of hepatotoxicity.[14] However, the quality of the evidence was judged to be low.[14] A shorter two-month course of rifampicin and pyrazinamide had previously been recommended, but is no longer due to high rates of hepatotoxicity.[15]
Rifampicin should be taken on an empty stomach with a glass of water. It is generally taken either at least one hour before meals or two hours after meals.[16]
Rifampicin is also used to treat non-tuberculous mycobacterial infections including leprosy (Hansen's disease) and Mycobacterium kansasii.[17]
With multidrug therapy used as the standard treatment of Hansen's disease, rifampicin is always used in combination with dapsone and clofazimine to avoid causing drug resistance.
Other bacteria and protozoans[edit]
Rifampicin is sometimes used in the treatment of methicillin-resistant Staphylococcus aureus (MRSA) in combination with fusidic acid, including in difficult-to-treat infections such as osteomyelitis and prosthetic joint infections.[18] It is also used as preventive treatment against Neisseria meningitidis (meningococcal) infections. Rifampicin is also recommended as an alternative treatment for infections by the tick-borne pathogens Borrelia burgdorferi and Anaplasma phagocytophilum when treatment with doxycycline is contraindicated, such as in pregnant women or in patients with a history of allergy to tetracycline antibiotics.[19][20]
It is also sometimes used to treat infections by Listeria species, Neisseria gonorrhoeae, Haemophilus influenzae, and Legionella pneumophila. For these nonstandard indications, antimicrobial susceptibility testing should be done (if possible) before starting rifampicin therapy.
The Enterobacteriaceae, Acinetobacter species, and Pseudomonas species are intrinsically resistant to rifampicin.
It has been used with amphotericin B in largely unsuccessful attempts to treat primary amoebic meningoencephalitis caused by Naegleria fowleri.
Rifampicin can be used as monotherapy for a few days as prophylaxis against meningitis, but resistance develops quickly during long-term treatment of active infections, so the drug is always used against active infections in combination with other antibiotics.[21]
Rifampicin is relatively ineffective against spirochetes, which has led to its use as a selective agent capable of isolating them in materials being cultured in laboratories.[22]
Viruses[edit]
Rifampicin has some effectiveness against vaccinia virus.[23][24]
Pathogen susceptibility[edit]
The following is information about minimum inhibitory concentrations of rifampicin for several medically significant pathogens:
- Mycobacterium tuberculosis — 0.002 – 64 µg/mL
- Mycobacterium bovis — 0.125 µg/mL
- Stapylococcus aureus (methicillin resistant) — ≤0.006–256 µg/mL[25]
- Chlamydia pneumoniae — 0.005 µg/mL[26]
Adverse effects[edit]
The most serious adverse effect is hepatotoxicity, and patients receiving it often undergo baseline and frequent liver function tests to detect early liver damage.
The more common side effects include fever, gastrointestinal disturbances, rashes, and immunological reactions. Taking rifampicin usually causes certain bodily fluids, such as urine, sweat, and tears, to become orange-red in color, a benign side effect that nonetheless can be frightening if it is not expected. This may also be used to monitor effective absorption of the drug (if drug color is not seen in the urine, the patient may wish to move the drug dose farther in time from food or milk intake). The discolorization of sweat and tears is not directly noticeable, but sweat may stain light clothing orange, and tears may permanently stain soft contact lenses. Since rifampicin may be excreted in breast milk, breast feeding should be avoided while it is being taken.
Other adverse effects include:
- Liver toxicity — hepatitis, liver failure in severe cases
- Respiratory — breathlessness
- Cutaneous — flushing, pruritus, rash, hyperpigmentation,[27] redness and watering of eyes
- Abdominal — nausea, vomiting, abdominal cramps, diarrhea
- Flu-like symptoms — chills, fever, headache, arthralgia, and malaise. Rifampicin has good penetration into the brain, and this may directly explain some malaise and dysphoria in a minority of users.
- Allergic reaction — rashes, itching, swelling of the tongue or throat, severe dizziness, and trouble breathing[28]
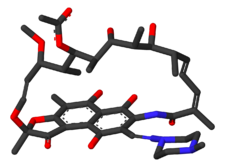
Chemical structure[edit]
Rifampicin belongs to the chemical class of compounds termed ansamycins, so named because of their heterocyclic structure containing a napthoquinone core spanned by an aliphatic ansa chain. The napthoquinonic chromophore is what gives rifampicin its characteristic red-orange crystalline color.
The critical functional groups of rifampicin in its inhibitory binding of bacterial RNA polymerase are the four critical hydroxyl groups of the ansa bridge and the napthol ring, which form hydrogen bonds with amino acid residues on the protein.[29]
Rifampicin is the 3-(4-methyl-1-piperazinyl)-iminomethyl derivative of rifamycin SV.[30]
Interactions[edit]
Rifampicin is the most powerful known inducer of the hepatic cytochrome P450 enzyme system, including isoenzymes CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP3A4, CYP3A5, and CYP3A7.[31] It increases metabolism of many drugs and as a consequence, can make them less effective, or even ineffective, by decreasing their levels.[32] For instance, patients undergoing long-term anticoagulation therapy with warfarin have to increase their dosage of warfarin and have their clotting time checked frequently because failure to do so could lead to inadequate anticoagulation, resulting in serious consequences of thromboembolism.[33]
Rifampicin can reduce the efficacy of birth control pills or other hormonal contraception by its induction of the cytochrome P450 system, to the extent that unintended pregnancies have occurred in women who use oral contraceptives and took rifampicin even for very short courses (for example, as prophylaxis against exposure to bacterial meningitis).
Other interactions include decreased levels and less effectiveness of antiretroviral agents, everolimus, atorvastatin, rosiglitazone, pioglitazone, celecoxib, clarithromycin, caspofungin, voriconazole, and lorazepam.[34]
Rifampicin is antagonistic to the microbiologic effects of the antibiotics gentamicin and amikacin.
Mechanism of action[edit]
Rifampicin inhibits bacterial DNA-dependent RNA synthesis by inhibiting bacterial DNA-dependent RNA polymerase.[35]
Crystal structure data and biochemical data suggest that rifampicin binds to the pocket of the RNA polymerase β subunit within the DNA/RNA channel, but away from the active site.[36] The inhibitor prevents RNA synthesis by physically blocking elongation, and thus preventing synthesis of host bacterial proteins. By this "steric-occlusion" mechanism, rifampicin blocks synthesis of the second or third phosphodiester bond between the nucleotides in the RNA backbone, preventing elongation of the 5' end of the RNA transcript past more than 2 or 3 nucleotides. [37][38]
Mechanism of resistance[edit]
Resistance to rifampicin arises from mutations that alter residues of the rifampicin binding site on RNA polymerase, resulting in decreased affinity for rifampicin.[38] Resistance mutations map to the rpoB gene, encoding the beta subunit of RNA polymerase. The majority of resistance mutations in E. coli are in 3 clusters on rpoB.[12] Cluster I is amino acids 509 to 533, cluster II is amino acids 563 to 572, and cluster III is amino acid 687.
When describing mutations in rpoB in other species, the corresponding amino acid number in E. coli is usually used. In Mycobacterium tuberculosis, the majority of mutations leading to rifampicin resistance are in cluster I, in a 81bp hotspot core region called RRDR for "rifampcin resistance determining region".[39] A change in amino acid 531 from serine to leucine arising from a change in the DNA sequence of TCG to TTG is the most common mutation.[12] Tuberculosis resistance has also occurred due to mutations in the N-terminal region of rpoB and cluster III.[12]
An alternative mechanism of resistance is through Arr-catalyzed ADP-ribosylation of rifampicin. With the assistance of the enzyme Arr produced by the pathogen Mycobacterium smegmatis, ADP-ribose is added to rifampicin at one of its ansa chain hydroxy groups, thereby inactivating the drug.[40]
Resistance in tuberculosis[edit]
Mycobacterial resistance to rifampicin may occur alone or along with resistance to other first line anti-tubercular drugs. Early detection of such multi-drug or extensively drug-resistant tuberculosis is critical in improving patient outcomes by instituting appropriate second-line treatments, and in decreasing transmission of drug-resistant TB.[41] Traditional methods of detecting resistance involve Mycobacterial culture and drug susceptibility testing, results of which could take up to six weeks. Xpert® MTB/RIF assay is an automated test that can detect rifampicin resistance, and also diagnose tuberculosis. A Cochrane review updated in 2014 concluded that for rifampicin resistance detection, Xpert® MTB/RIF was accurate, that is (95%) sensitive and (98%) specific.[42]
Pharmacokinetics[edit]
Orally administered rifampicin results in peak plasma concentrations in about two to four hours. 4-Aminosalicylic acid (another antituberculosis drug) significantly reduces absorption of rifampicin,[43] and peak concentrations may be lower. If these two drugs must be used concurrently, they must be given separately, with an interval of eight to 12 hours between administrations.
Rifampicin is easily absorbed from the gastrointestinal tract; its ester functional group is quickly hydrolyzed in bile, and it is catalyzed by a high pH and substrate-specific esterases. After about six hours, almost all of the drug is deacetylated. Even in this deacetylated form, rifampicin is still a potent antibiotic; however, it can no longer be reabsorbed by the intestines and is eliminated from the body. Only about 7% of the administered drug is excreted unchanged in urine, though urinary elimination accounts for only about 30% of the drug excretion. About 60% to 65% is excreted through feces.
The half-life of rifampicin ranges from 1.5 to 5.0 hours, though hepatic impairment significantly increases it. Food consumption inhibits its absorption from the GI tract, and the drug is more quickly eliminated. When rifampicin is taken with a meal, its peak blood concentration falls by 36%. Antacids do not affect its absorption.[44] The decrease in rifampicin absorption with food is sometimes enough to noticeably affect urine color, which can be used as a marker for whether or not a dose of the drug has been effectively absorbed.
Distribution of the drug is high throughout the body, and reaches effective concentrations in many organs and body fluids, including the cerebrospinal fluid. Since the substance itself is red, this high distribution is the reason for the orange-red color of the saliva, tears, sweat, urine, and feces. About 60% to 90% of the drug is bound to plasma proteins.[45]
Use in biotechnology[edit]
Rifampicin inhibits bacterial RNA polymerase, thus it is commonly used to inhibit the synthesis of host bacterial proteins during recombinant protein expression in bacteria. RNA encoding for the recombinant gene is usually transcribed from DNA by a viral T7 RNA polymerase, which is not affected by rifampicin.
History[edit]
In 1957, a soil sample from a pine forest on the French Riviera was brought for analysis to the Lepetit Pharmaceuticals research lab in Milan, Italy. There, a research group headed by Piero Sensi[46] and Maria Teresa Timbal discovered a new bacterium. This new species produced a new class of molecules with antibiotic activity. Because Sensi, Timbal and the researchers were particularly fond of the French crime story Rififi (about a jewel heist and rival gangs),[47] they decided to call these compounds "rifamycins". After two years of attempts to obtain more stable semisynthetic products, a new molecule with high efficacy and good tolerability was produced in 1965 and was named "rifampicin".[3]
Rifampicin was first sold in Italy in 1968 and was approved by the FDA in 1971.[3]
Names[edit]
Rifampicin is the INN and BAN while rifampin is the USAN. Rifampicin may be abbreviated R, RMP, RA, RF, or RIF (US).
Rifampicin is also known as rifaldazine,[48][49] rofact, and rifampin in the United States, also as rifamycin SV.[50]
Its chemical name is 5,6,9,17,19,21-hexahydroxy-23-methoxy-2,4,12,16,18,20,22-heptamethyl-8-[N-(4-methyl-1-piperazinyl)formimidoyl]-2,7-(epoxypentadeca[1,11,13]trienimino)-naphtho[2,1-b]furan-1,11(2H)-dione 21-acetate
Rifampicin is available under many brand names worldwide.[51]
References[edit]
- ^ "Rifampicin (CAS 13292-46-1)". Santa Cruz Biotechnology Product Block. Santa Cruz Biotechnology. Retrieved 14 November 2014.
- ^ a b c d e "Rifampin". The American Society of Health-System Pharmacists. Retrieved Aug 1, 2015.
- ^ a b c Sensi, P (1983). "History of the development of rifampin". Reviews of Infectious Diseases. 5 Suppl 3: S402–6. doi:10.1093/clinids/5.supplement_3.s402. JSTOR 4453138. PMID 6635432.
- ^ Oxford Handbook of Infectious Diseases and Microbiology. OUP Oxford. 2009. p. 56. ISBN 978-0-19-103962-1.
- ^ a b McHugh, Timothy D. (2011). Tuberculosis: diagnosis and treatment. Wallingford, Oxfordshire: CAB International. p. 219. ISBN 978-1-84593-807-9.
- ^ "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Retrieved 8 December 2016.
- ^ "Rifampicin". International Drug Price Indicator Guide. Retrieved 24 August 2015.
- ^ Hamilton, Richard J. (2014). Tarascon pocket pharmacopoeia: 2014 deluxe lab-pocket edition (15 ed.). Sudbury: Jones & Bartlett Learning. p. 39. ISBN 978-1-284-05399-9.
- ^ "Treatment of tuberculosis: guidelines". World Health Organization. 2010. ISBN 978-92-4-154783-3.
- ^ Long, James W. (1991). Essential Guide to Prescription Drugs 1992. New York: HarperCollins Publishers. pp. 925–929. ISBN 0-06-273090-8.
- ^ Erlich, Henry, W Ford Doolittle, Volker Neuhoff, et al. Molecular Biology of Rifamycin. New York, NY: MSS Information Corporation, 1973. pp. 44-45, 66-75, 124-130.
- ^ a b c d Goldstein, Beth P. "Resistance to rifampicin: a review". The Journal of Antibiotics. 67 (9): 625–630. doi:10.1038/ja.2014.107.
- ^ David HL (1970). "Probability Distribution of Drug-Resistant Mutants in Unselected Populations of Mycobacterium tuberculosis". Appl Microbiol. 20: 810–4. PMC 377053
 . PMID 4991927.
. PMID 4991927. - ^ a b Sharma, SK; Sharma, A; Kadhiravan, T; Tharyan, P (July 5, 2013). "Rifamycins (rifampicin, rifabutin and rifapentine) compared to isoniazid for preventing tuberculosis in HIV-negative people at risk of active TB". The Cochrane Database of Systematic Reviews. 7: CD007545. doi:10.1002/14651858.CD007545.pub2. PMID 23828580.
- ^ "Update: adverse event data and revised American Thoracic Society/CDC recommendations against the use of rifampin and pyrazinamide for treatment of latent tuberculosis infection - United States, 2003". MMWR Morbidity and Mortality Weekly Report. 52 (31): 735–739. 2003-08-08. ISSN 1545-861X. PMID 12904741.
- ^ "Rifampin oral: Uses, Side Effects, Interactions, Pictures, Warnings & Dosing – WebMD". WebMD. WebMD. Retrieved 13 November 2014.
- ^ The Sanford Guide to Antimicrobial Therapy 2015. ISBN 978-1-930808-84-3.
- ^ Aboltins CA, Page MA, Buising KL, et al. (June 2007). "Treatment of staphylococcal prosthetic joint infections with debridement, prosthesis retention and oral rifampicin and fusidic acid". Clinical Microbiology and Infection. 13 (6): 586–591. doi:10.1111/j.1469-0691.2007.01691.x. PMID 17331125.
- ^ Wormser, Gary P.; Dattwyler, Raymond J.; Shapiro, Eugene D.; Halperin, John J.; Steere, Allen C.; Klempner, Mark S.; Krause, Peter J.; Bakken, Johan S.; Strle, Franc; Stanek, Gerold; Bockenstedt, Linda; Fish, Durland; Stephen Dumler, J.; Nadelman, Robert B. (1 November 2006). "The Clinical Assessment, Treatment, and Prevention of Lyme Disease, Human Granulocytic Anaplasmosis, and Babesiosis: Clinical Practice Guidelines by the Infectious Diseases Society of America". Clinical Infectious Diseases. 43 (9): 1089–1134. doi:10.1086/508667. PMID 17029130.
- ^ Thomas RG, Dumler SJ, Carlyon JA (August 2009). "Current management of human granulocytic anaplasmosis, human monocytic ehrlichiosis and Ehrlichia ewingii ehrlichiosis". Expert Reviews in Anti-Infection Therapies. 7 (6): 709–722. doi:10.1586/eri.09.44. PMC 2739015
 . PMID 19681699.
. PMID 19681699. - ^ "Rifampicin". Retrieved August 22, 2014.
- ^ Leschine, S.B.; Canale-Parola, E. (December 1980). "Rifampin as a Selective Agent for the Isolation of Oral Spirochetes" (PDF). Journal of Clinical Microbiology. 12 (6): 792–795. PMC 273700
 . PMID 7309842. Retrieved 3 March 2016.
. PMID 7309842. Retrieved 3 March 2016. - ^ Charity JC, Katz E, Moss B (March 2007). "Amino acid substitutions at multiple sites within the vaccinia virus D13 scaffold protein confer resistance to rifampicin". Virology. 359 (1): 227–32. doi:10.1016/j.virol.2006.09.031. PMC 1817899
 . PMID 17055024.
. PMID 17055024. - ^ Sodeik B, Griffiths G, Ericsson M, Moss B, Doms RW (February 1994). "Assembly of vaccinia virus: effects of rifampin on the intracellular distribution of viral protein p65". Journal of Virology. 68 (2): 1103–14. PMC 236549
 . PMID 8289340.
. PMID 8289340. - ^ "Rifampicin (Rifampin) - The Antimicrobial Index Knowledgebase - TOKU-E". toku-e.com.
- ^ Gieffers J, Solbach W, Maass M (1998). "Note: In Vitro Susceptibilities of Chlamydia pneumoniae Strains Recovered from Atherosclerotic Coronary Arteries". Antimicrobial Agents and Chemotherapy. 42: 2762–4. PMC 105936
 . PMID 9756794.
. PMID 9756794. - ^ Pugazhenthan Thangaraju; Hosanna Singh; M Punitha; VC Giri; MK Showkath Ali. (2015). "Hyperpigmentation, a marker of rifampicin overuse in leprosy patient: An incidental finding". Sudan Med Monitor. 10 (1): 25–26. doi:10.4103/1858-5000.157506.
- ^ "Rifampin oral: Uses, Side Effects, Interactions, Pictures, Warnings & Dosing – WebMD". WebMD. WebMD. Retrieved 13 November 2014.
- ^ Campbell, Elizabeth A.; Korzheva, Nataliya; Mustaev, Arkady; Murakami, Katsuhiko; Nair, Satish; Goldfarb, Alex; Darst, Seth A. (March 2001). "Structural Mechanism for Rifampicin Inhibition of Bacterial RNA Polymerase". Cell. 104 (6): 901–912. doi:10.1016/s0092-8674(01)00286-0. PMID 11290327.
- ^ Bennett, John (2015). Principles and Practice of Infectious Diseases. Elsevier Health Sciences. p. 339.
- ^ "Division of Clinical Pharmacology | Indiana University Department of Medicine". Medicine.iupui.edu. 2011-09-27. Retrieved 2011-11-07.
- ^ Collins, R Douglas. Atlas of Drug Reactions. New York, NY: ChurchillLivingstone, 1985. pp. 123.
- ^ Stockley, Ivan H. "Anticoagulant Drug Interactions." Drug Interactions. 3rd ed. Boston: Blackwell Scientific Publications, 1994. pp. 274-275.
- ^ Riss, J.; Cloyd, J.; Gates, J.; Collins, S. (August 2008). "Benzodiazepines in epilepsy: pharmacology and pharmacokinetics". Acta Neurologica Scandinavica. 118 (2): 69–86. doi:10.1111/j.1600-0404.2008.01004.x. PMID 18384456.
- ^ Calvori, C.; Frontali, L.; Leoni, L.; Tecce, G. (1965). "Effect of rifamycin on protein synthesis". Nature. 207 (995): 417–8. doi:10.1038/207417a0. PMID 4957347.
- ^ Campbell, Elizabeth A.; Korzheva, Nataliya; Mustaev, Arkady; Murakami, Katsuhiko; Nair, Satish; Goldfarb, Alex; Darst, Seth A. (March 2001). "Structural Mechanism for Rifampicin Inhibition of Bacterial RNA Polymerase". Cell. 104 (6): 901–912. doi:10.1016/s0092-8674(01)00286-0. PMID 11290327.
- ^ Campbell, E.A., Korzheva, N., Mustaev, A., Murakami, K., Nair, S., Goldfarb, A., Darst, S.A. (2001). "Structural mechanism for rifampicin inhibition of bacterial RNA polymerase". Cell. 104 (6): 901–12. doi:10.1016/S0092-8674(01)00286-0. PMID 11290327.
- ^ a b Feklistov, A., Mekler, V., Jiang, Q., Westblade, L.F., Irschik, H., Jansen, R., Mustaev, A., Darst, S.A., Ebright, R.H. (2008). "Rifamycins do not function by allosteric modulation of binding of Mg2+ to the RNA polymerase active center". Proceedings of the National Academy of Sciences – USA. 105 (39): 14820–5. doi:10.1073/pnas.0802822105. PMC 2567451
 . PMID 18787125.
. PMID 18787125. - ^ Pierre-Audiger, C.; Gicquel, B. "The Contribution of Molecular Biology in Diagnosing Tuberculosis and Detecting Antibiotic Resistance" (PDF). Molecular TB.
- ^ Baysarowich, Jennifer; Koteva, Kalinka; Hughes, Donald W.; Ejim, Linda; Griffiths, Emma; Zhang, Kun; Junop, Murray; Wright, Gerard D. (2008-03-25). "Rifamycin antibiotic resistance by ADP-ribosylation: Structure and diversity of Arr". Proceedings of the National Academy of Sciences. 105 (12): 4886–4891. doi:10.1073/pnas.0711939105. ISSN 0027-8424. PMC 2290778
 . PMID 18349144.
. PMID 18349144. - ^ Policy Framework for Implementing New Tuberculosis Diagnostics (PDF). Geneva: World Health Organization. 2011. Retrieved 21 March 2016.
- ^ Steingart, KR; Schiller, I; Horne, DJ; Pai, M; Boehme, CC; Dendukuri, N (21 January 2014). "Xpert® MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults". The Cochrane Database of Systematic Reviews. 1: CD009593. doi:10.1002/14651858.CD009593.pub3. PMC 4470349
 . PMID 24448973. Retrieved 21 March 2016.
. PMID 24448973. Retrieved 21 March 2016. - ^ G Curci, A Ninni, A.D'Aleccio (1969) Atti Tavola Rotonda Rifampicina, Taormina, page 19. Edizioni Rassegna Medica, Lepetit, Milano
- ^ "Kinetics of Rifampin taken with food and with antacids" (PDF). Retrieved 2011-11-07.
- ^ Hardman, Joel G., Lee E. Limbird, and Alfred G. Gilman, eds. "Rifampin." The Pharmacological Basis of Therapeutics. 10th ed. United States of America: The McGraw-Hill Companies, 2001. pp. 1277–1279.
- ^ "Il chimico che salvò molte vite". corriere.it.
- ^ "When I Use a Word . . .I Mean It". British Medical Journal 1999;319(7215):972 (9 October). Retrieved 2009-07-10.
- ^ Moncalvo F, Moreo G (1966). "Ricerche cliniche preliminari sull'impiego di una nuova rifamicina orale (rifaldazina) nella terapia della tubercolosi polmonare (nota preventiva)". Giornale Italiano Della Tubercolosi E Delle Malattie Del Torace. 20 (3): 120–31. PMID 5974175.
- ^ "Rifampicin". Chemical Safety Information from Intergovernmental Organizations. International Programme on Chemical Safety. Retrieved 14 November 2014.
- ^ "US Patent 3963705" (Patent). Google. US Patent Office. Retrieved 14 November 2014.
- ^ Drugs.com international listings for Rifampicin. Accessed Jan 15 2015

