Sirolimus
 |
|
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
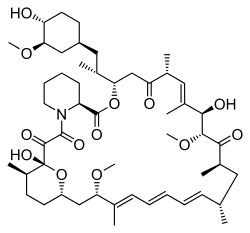
(3S,6R,7E,9R,10R,12R,14S,15E,17E,19E,21S,23S,
26R,27R,34aS)-9,10,12,13,14,21,22,23,24,25,26, 27,32,33,34,34a-hexadecahydro-9,27-dihydroxy-3- [(1R)-2-[(1S,3R,4R)-4-hydroxy-3-methoxycyclohexyl]- 1-methylethyl]-10,21-dimethoxy-6,8,12,14,20,26- hexamethyl-23,27-epoxy-3H-pyrido[2,1-c][1,4]- oxaazacyclohentriacontine-1,5,11,28,29 (4H,6H,31H)-pentone |
|
| Clinical data | |
| Trade names | Rapamune |
| License data | |
| Pregnancy category |
|
| Routes of administration |
Oral |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 14% (oral solution), lower with high-fat meals; 18% (tablet), higher with high-fat meals[1] |
| Protein binding | 92% |
| Metabolism | Hepatic |
| Biological half-life | 57–63 hours |
| Excretion | Mostly faecal |
| Identifiers | |
| CAS Number | 53123-88-9 |
| ATC code | L04AA10 (WHO) S01XA23 (WHO) |
| PubChem | CID 5284616 |
| DrugBank | DB00877 |
| ChemSpider | 10482078 |
| UNII | W36ZG6FT64 |
| KEGG | D00753 |
| ChEBI | CHEBI:9168 |
| ChEMBL | CHEMBL413 |
| Synonyms | Rapamycin |
| PDB ligand ID | RAP (PDBe, RCSB PDB) |
| Chemical data | |
| Formula | C51H79NO13 |
| Molar mass | 914.172 g/mol |
|
|
|
|
| Physical data | |
| Solubility in water | 0.0026 [2] mg/mL (20 °C) |
| |
|
Sirolimus (INN/USAN), also known as rapamycin, is a macrolide (one of a group of drugs containing a macrolide ring) produced by the bacterium Streptomyces hygroscopicus.[3] It has immunosuppressant functions in humans and is used to prevent rejection in organ transplantation; it is especially useful in kidney transplants. It prevents activation of T cells and B cells by inhibiting the production of interleukin-2 (IL-2). Sirolimus is also used as a coronary stent coating.
Sirolimus was isolated for the first time in 1972 by Suren Sehgal and colleagues from samples of Streptomyces hygroscopicus found on Easter Island.[4][5] The compound was originally named rapamycin after the native name of the island, Rapa Nui.[3] Sirolimus was initially developed as an antifungal agent. However, this use was abandoned when it was discovered to have potent immunosuppressive and antiproliferative properties due to its ability to inhibit mTOR. It was approved by the US Food and Drug Administration in September 1999 and is marketed under the trade name Rapamune by Pfizer (formerly by Wyeth).
Contents
Mechanism of action[edit]
Unlike the similarly named tacrolimus, sirolimus is not a calcineurin inhibitor, but it has a similar suppressive effect on the immune system. Sirolimus inhibits IL-2 and other cytokines receptor-dependent signal transduction mechanisms, via action on mTOR, and thereby blocks activation of T and B cells. Tacrolimus and cyclosporine inhibit the secretion of IL-2, by inhibiting calcineurin.
The mode of action of sirolimus is to bind the cytosolic protein FK-binding protein 12 (FKBP12) in a manner similar to tacrolimus. Unlike the tacrolimus-FKBP12 complex, which inhibits calcineurin (PP2B), the sirolimus-FKBP12 complex inhibits the mTOR (mechanistic (formerly mammalian) Target Of Rapamycin, rapamycin being another name for sirolimus) pathway by directly binding to mTOR Complex 1 (mTORC1).
mTOR has also been called FRAP (FKBP-rapamycin-associated protein), RAFT (rapamycin and FKBP target), RAPT1, or SEP. The earlier names FRAP and RAFT were coined to reflect the fact that sirolimus must bind FKBP12 first, and only the FKBP12-sirolimus complex can bind mTOR. However, mTOR is now the widely accepted name, since Tor was first discovered via genetic and molecular studies of sirolimus-resistant mutants of Saccharomyces cerevisiae that identified FKBP12, Tor1, and Tor2 as the targets of sirolimus and provided robust support that the FKBP12-sirolimus complex binds to and inhibits Tor1 and Tor2.
Clinical uses[edit]
Prevention of transplant rejection[edit]
The chief advantage sirolimus has over calcineurin inhibitors is its low toxicity toward kidneys. Transplant patients maintained on calcineurin inhibitors long-term tend to develop impaired kidney function or even chronic renal failure; this can be avoided by using sirolimus instead. It is particularly advantageous in patients with kidney transplants for hemolytic-uremic syndrome, as this disease is likely to recur in the transplanted kidney if a calcineurin-inhibitor is used. However, on October 7, 2008, the FDA approved safety labeling revisions for sirolimus to warn of the risk for decreased renal function associated with its use.
Sirolimus can also be used alone, or in conjunction with calcineurin inhibitors, such as tacrolimus and/or mycophenolate mofetil, to provide steroid-free immunosuppression regimens. Impaired wound healing and thrombocytopenia are a possible side effects of sirolimus; therefore, some transplant centres prefer not to use it immediately after the transplant operation, but instead administer it only after a period of weeks or months. Its optimal role in immunosuppression has not yet been determined, and it remains the subject of a number of ongoing clinical trials.
The absorption of sirolimus into the blood stream from the intestine varies widely between patients, with some patients having up to eight times more exposure than others for the same dose. Drug levels are, therefore, taken to make sure patients get the right dose for their condition. This is determined by taking a blood sample before the next dose, which gives the trough level. However, good correlation is noted between trough concentration levels and drug exposure, known as area under the concentration-time curve, for both sirolimus (SRL) and tacrolimus (TAC) (SRL: r2 = 0.83; TAC: r2 = 0.82), so only one level need be taken to know its pharmacokinetic (PK) profile. PK profiles of SRL and of TAC are unaltered by simultaneous administration. Dose-corrected drug exposure of TAC correlates with SRL (r2 = 0.8), so patients have similar bioavailability of both.[6]
Coronary stent coating[edit]
The antiproliferative effect of sirolimus has also been used in conjunction with coronary stents to prevent restenosis in coronary arteries following balloon angioplasty. The sirolimus is formulated in a polymer coating that affords controlled release through the healing period following coronary intervention. Several large clinical studies have demonstrated lower restenosis rates in patients treated with sirolimus-eluting stents when compared to bare-metal stents, resulting in fewer repeat procedures. A sirolimus-eluting coronary stent was marketed by Cordis, a division of Johnson & Johnson, under the tradename Cypher.[7] However, this kind of stent may also increase the risk of vascular thrombosis.[8]
Lymphangioleiomyomatosis[edit]
Sirolimus is indicated for the treatment of lymphangioleiomyomatosis (LAM).[9]
Adverse effects[edit]
The most common adverse reactions (≥30% occurrence, leading to a 5% treatment discontinuation rate) observed with sirolimus in clinical studies of organ rejection prophylaxis in individuals with kidney transplants include: peripheral edema, hypercholesterolemia, abdominal pain, headache, nausea, diarrhea, pain, constipation, hypertriglyceridemia, hypertension, increased creatinine, fever, urinary tract infection, anemia, arthralgia, and thrombocytopenia.[9]
The most common adverse reactions (≥20% occurrence, leading to a 11% treatment discontinuation rate) observed with sirolimus in clinical studies for the treatment of lymphangioleiomyomatosis are: peripheral edema, hypercholesterolemia, abdominal pain, headache, nausea, diarrhea, chest pain, stomatitis, nasopharyngitis, acne, upper respiratory tract infection, dizziness, and myalgia.[9]
The following adverse effects occurred in 3–20% of individuals taking sirolimus for organ rejection prophylaxis following a kidney transplant:[9]
| System | Adverse effects |
|---|---|
| Body as a Whole | Sepsis, lymphocele, herpes zoster infection, herpes simplex infection |
| Cardiovascular | Venous thromboembolism (pulmonary embolism and deep venous thrombosis), rapid heart rate |
| Digestive | Stomatitis |
| Hematologic/Lymphatic | Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS), leukopenia |
| Metabolic | Abnormal healing, increased lactic dehydrogenase (LDH), hypokalemia, diabetes |
| Musculoskeletal | Bone necrosis |
| Respiratory | Pneumonia, epistaxis |
| Skin | Melanoma, squamous cell carcinoma, basal cell carcinoma |
| Urogenital | Pyelonephritis, ovarian cysts, menstrual disorders (amenorrhea and menorrhagia) |
Diabetes-like symptoms[edit]
While sirolimus inhibition of mTORC1 appears to mediate the drug's benefits, it also inhibits mTORC2, which results in diabetes-like symptoms. This includes decreased glucose tolerance and insensitivity to insulin.[10] Sirolimus treatment may additionally increase the risk of type 2 diabetes.[11] In mouse studies, these symptoms can be avoided through the use of alternate dosing regimens or analogs such as everolimus or temsirolimus.[12]
Lung toxicity[edit]
Lung toxicity is a serious complication associated with sirolimus therapy,[13][14][15][16][17][18][19] especially in the case of lung transplants.[20] The mechanism of the interstitial pneumonitis caused by sirolimus and other macrolide MTOR inhibitors is unclear, and may have nothing to do with the mTOR pathway.[21][22][23] The interstitial pneumonitis is not dose-dependent, but is more common in patients with underlying lung disease.[13][24]
Lowered effectiveness of immune system[edit]
There have been warnings about the use of sirolimus in transplants, where it may increase mortality due to an increased risk of infections.[9][25]
Cancer risk[edit]
According to FDA prescribing information, sirolimus may increase an individual's risk for contracting skin cancers from exposure to sunlight or UV radiation, and risk of developing lymphoma.[9]
Impaired wound healing[edit]
Individuals taking sirolimus are at increased risk of experiencing impaired or delayed wound healing, particularly if they have a high body mass index (i.e., a BMI of ≥30 kg/m2).[9]
Biosynthesis[edit]
The biosynthesis of the rapamycin core is accomplished by a type I polyketide synthase (PKS) in conjunction with a nonribosomal peptide synthetase (NRPS). The domains responsible for the biosynthesis of the linear polyketide of rapamycin are organized into three multienzymes, RapA, RapB, and RapC, which contain a total of 14 modules (figure 1). The three multienzymes are organized such that the first four modules of polyketide chain elongation are in RapA, the following six modules for continued elongation are in RapB, and the final four modules to complete the biosynthesis of the linear polyketide are in RapC.[26] Then, the linear polyketide is modified by the NRPS, RapP, which attaches L-pipecolate to the terminal end of the polyketide, and then cyclizes the molecule, yielding the unbound product, prerapamycin.[27]
The core macrocycle, prerapamycin (figure 2), is then modified (figure 3) by an additional five enzymes, which lead to the final product, rapamycin. First, the core macrocycle is modified by RapI, SAM-dependent O-methyltransferase (MTase), which O-methylates at C39. Next, a carbonyl is installed at C9 by RapJ, a cytochrome P-450 monooxygenases (P-450). Then, RapM, another MTase, O-methylates at C16. Finally, RapN, another P-450, installs a hydroxyl at C27 immediately followed by O-methylation by Rap Q, a distinct MTase, at C27 to yield rapamycin.[28]
The biosynthetic genes responsible for rapamycin synthesis have been identified. As expected, three extremely large open reading frames (ORF's) designated as rapA, rapB, and rapC encode for three extremely large and complex multienzymes, RapA, RapB, and RapC, respectively.[26] The gene rapL has been established to code for a NAD+-dependent lysine cycloamidase, which converts L-lysine to L-pipecolic acid (figure 4) for incorporation at the end of the polyketide.[29][30] The gene rapP, which is embedded between the PKS genes and translationally coupled to rapC, encodes for an additional enzyme, an NPRS responsible for incorporating L-pipecolic acid, chain termination and cyclization of prerapamycin. In addition, genes rapI, rapJ, rapM, rapN, rapO, and rapQ have been identified as coding for tailoring enzymes that modify the macrocyclic core to give rapamycin (figure 3). Finally, rapG and rapH have been identified to code for enzymes that have a positive regulatory role in the preparation of rapamycin through the control of rapamycin PKS gene expression.[31] Biosynthesis of this 31-membered macrocycle begins as the loading domain is primed with the starter unit, 4,5-dihydroxocyclohex-1-ene-carboxylic acid, which is derived from the shikimate pathway.[26] Note that the cyclohexane ring of the starting unit is reduced during the transfer to module 1. The starting unit is then modified by a series of Claisen condensations with malonyl or methylmalonyl substrates, which are attached to an acyl carrier protein (ACP) and extend the polyketide by two carbons each. After each successive condensation, the growing polyketide is further modified according to enzymatic domains that are present to reduce and dehydrate it, thereby introducing the diversity of functionalities observed in rapamycin (figure 1). Once the linear polyketide is complete, L-pipecolic acid, which is synthesized by a lysine cycloamidase from an L-lysine, is added to the terminal end of the polyketide by an NRPS. Then, the NSPS cyclizes the polyketide, giving prerapamycin, the first enzyme-free product. The macrocyclic core is then customized by a series of post-PKS enzymes through methylations by MTases and oxidations by P-450s to yield rapamycin.
Research[edit]

Cancer[edit]
The antiproliferative effects of sirolimus may have a role in treating cancer. When dosed appropriately, sirolimus can enhance the immune response to tumor targeting[32] or otherwise promote tumor regression in clinical trials.[33] Sirolimus seems to lower the cancer risk in some transplant patients.[34]
Sirolimus was shown to inhibit the progression of dermal Kaposi's sarcoma in patients with renal transplants. Other mTOR inhibitors, such as temsirolimus (CCI-779) or everolimus (RAD001), are being tested for use in cancers such as glioblastoma multiforme and mantle cell lymphoma. However, these drugs have a higher rate of fatal adverse events in cancer patients than control drugs.[35]
A combination therapy of doxorubicin and sirolimus has been shown to drive AKT-positive lymphomas into remission in mice. Akt signalling promotes cell survival in Akt-positive lymphomas and acts to prevent the cytotoxic effects of chemotherapy drugs, such as doxorubicin or cyclophosphamide. Sirolimus blocks Akt signalling and the cells lose their resistance to the chemotherapy. Bcl-2-positive lymphomas were completely resistant to the therapy; eIF4E-expressing lymphomas are not sensitive to sirolimus.[36][37][38][39]
Tuberous sclerosis complex[edit]
Sirolimus also shows promise in treating tuberous sclerosis complex (TSC), a congenital disorder that leaves sufferers prone to benign tumor growth in the brain, heart, kidneys, skin, and other organs. After several studies conclusively linked mTOR inhibitors to remission in TSC tumors, specifically subependymal giant-cell astrocytomas in children and angiomyolipomas in adults, many US doctors began prescribing sirolimus (Wyeth's Rapamune) and everolimus (Novartis's RAD001) to TSC patients off-label. Numerous clinical trials using both rapamycin analogs, involving both children and adults with TSC, are underway in the United States.[40]
Most studies thus far have noted that tumors often regrew when treatment stopped. Theories that claim the drug ameliorates TSC symptoms such as facial angiofibromas and autism are a matter of current research in animal models.[medical citation needed]
Effects on longevity[edit]
Rapamycin was first shown to extend lifespan in eukaryotes in 2006.[41] Powers et al. showed a dose-responsive effect of rapamycin on lifespan extension in yeast cells. Building on this and other work, in a 2009 study, the lifespans of mice fed rapamycin were increased between 28 and 38% from the beginning of treatment, or 9 to 14% in total increased maximum lifespan. Of particular note, the treatment began in mice aged 20 months, the equivalent of 60 human years. This suggests the possibility of an effective antiaging treatment for humans at an already-advanced age, as opposed to requiring a lifelong regimen beginning in youth.[42] Rapamycin has subsequently been shown to extend mouse lifespan in several separate experiments,[43][44] and is now being tested for this purpose in nonhuman primates (the marmoset monkey),[45] and with an ongoing attempt to organize a study in dogs.[46] The Dog Aging Project is funded by pet owners.[47]
Because rapamycin at high doses can suppress the immune system, people taking rapamycin for transplant or cancer therapy are more susceptible to dangerous infections. Yet paradoxically, rapamycin was shown to enhance the ability of aging mice to mount an immune response to a vaccine against tuberculosis.[48] A similar immunological "rejuvenating" effect was later documented in elderly humans administered a rapamycin analog prior to influenza vaccination),[49] further fueling optimism for the potential of mTOR as a target for anti-aging drugs for humans. Recent work in mice suggests that intermittent treatment with rapamycin may substantially reduce side effects while still promoting health and extending lifespan.[50][51][52][53][54][55] Co-administration of the anti-diabetes drug metformin may further increase the lifespan of rapamycin-treated mice.[56]
However, it is not known whether rapamycin will have similar lifespan-lengthening effects in humans, and study authors caution that the drug should not be used by the general population for this use.[57]
Decreased TOR activity has been found to increase life span in S. cerevisiae, C. elegans, and D. melanogaster.[58][59][60][61] The mTOR inhibitor rapamycin has been confirmed to increase lifespan in mice.[62][63][64]
It is hypothesized that some dietary regimes, like caloric restriction and methionine restriction, cause lifespan extension by decreasing mTOR activity.[58][59] It is believed that this is achieved by limiting the essential amino acid leucine, a potent activator of mTOR.[citation needed] The administration of leucine into the rat brain has been shown to decrease food intake and body weight via activation of the mTOR pathway.[65]
According to the free radical theory of aging,[66] reactive oxygen species cause damage of mitochondrial proteins and decrease of ATP production. Subsequently, via ATP sensitive AMPK, the mTOR pathway is inhibited and ATP consuming protein synthesis is downregulated, since mTORC1 initiates a phosphorylation cascade activating the ribosome.[67] Hence, the proportion of damaged proteins is enhanced. Moreover, disruption of mTORC1 directly inhibits mitochondrial respiration.[68] These positive feedbacks on the aging process are counteracted by protective mechanisms: Decreased mTOR activity (among other factors) upregulates glycolysis[68] and removal of dysfunctional cellular components via autophagy.[66]
Tuberous sclerosis in mice, with possible relevance to autism[edit]
In a study of sirolimus as a treatment for tuberous sclerosis, researchers observed improvements in TSC symptoms which overlap with autism. The researchers discovered that sirolimus regulates one of the same proteins the TSC gene does, but in different parts of the body. They decided to treat mice three to six months old (adulthood in mice lifespans); this increased the TSC mice's intellect to about that of normal mice in as little as three days.[69]
Alzheimer's in mice[edit]
Sirolimus reduced brain lesions and prevented the decline of performance in the water maze in mice with a mouse model of Alzheimer's.[70] Recent studies have observed a protective effect against Alzheimer's Disease in preventing cognitive deficits and reducing amyloid-β levels in mouse models. [71]
Muscular dystrophy in mice[edit]
Researchers at Washington University School of Medicine in St. Louis observed that nanoparticles coated in sirolimus increases grip strength by 30% and significantly increases cardiac function in mice. The nanoparticle consists of a core of perfluorocarbon and are 200 nm in diameter. The nanoparticle accumulates in areas of inflammation, in this case the muscles where it releases a small dose of sirolimus. This suppresses the immune system and promotes autophagy.[72]
Systemic lupus erythematosus in mice and humans[edit]
Sirolimus improves disease activity and dependence on prednisone in systemic lupus erythematosus (SLE) patients resistant or intolerant to immunosuppressant medications. Sirolimus acts through blocking the activation of its molecular target, the mechanistic target of rapamycin complex 1 (mTORC1). The activation of mTORC1, which is associated with suppression of mTORC2, results in the expansion of proinflammatory CD4-CD8- double-negative (DN) T lymphocytes. These DN T cells produce inflammatory cytokines, interleukin-4 (IL-4) and interleukin-17, and they exhibit predisposition to proinflammatory cell death through necrosis. Increased IL-4 production is responsible for activation of autoantibody-producing B lymphocytes in SLE.[73][74][75][76][77] Sirolimus also blocks disease in lupus-prone mice by reversing the activation of mTORC1.[78] Prospective clinical trial in SLE patients with sirolimus is ongoing.
Other afflictions[edit]
Studies in vitro in mice and in humans suggest sirolimus inhibits HIV replication through different mechanisms, including downregulation of the coreceptor CCR5[79] and the induction of autophagy.[80]
In addition, sirolimus is currently being assessed as a therapeutic option for autosomal-dominant polycystic kidney disease (ADPKD). Case reports indicate sirolimus can reduce kidney volume and delay the loss of renal function in patients with ADPKD.[81]
Sirolimus has also been used in preliminary research to combat progeria, a rare disorder that causes individuals to age at an exceedingly rapid pace, leading to an extremely compromised cell-damage repair capacity and typically resulting in death in the early teenage years due to causes which are generally associated with old age such as heart disease or stroke.[82]
Applications in biology research[edit]
Rapamycin is used in biology research as an agent for chemically induced dimerization.[83] In this application, rapamycin is added to cells expressing two fusion constructs, one of which contains the rapamycin-binding FRB domain from mTOR and the other of which contains an FKBP domain. Each fusion protein also contains additional domains that are brought into proximity when rapamycin induces binding of FRB and FKBP. In this way, rapamycin can be used to control and study protein localization and interactions.
References[edit]
- ^ Buck, Marcia L. (2006). "Immunosuppression With Sirolimus After Solid Organ Transplantation in Children". Pediatric Pharmacotherapy 12 (2).
- ^ Simamora, P; Alvarez, JM; Yalkowsky, SH (1 February 2001). "Solubilization of rapamycin". International journal of pharmaceutics 213 (1-2): 25–9. doi:10.1016/s0378-5173(00)00617-7. PMID 11165091.
- ^ a b Vézina C, Kudelski A, Sehgal SN (October 1975). "Rapamycin (AY-22,989), a new antifungal antibiotic". J. Antibiot. 28 (10): 721–6. doi:10.7164/antibiotics.28.721. PMID 1102508.
- ^ Seto, Belinda (2012). "Rapamycin and mTOR: a serendipitous discovery and implications for breast cancer". Clinical and Translational Medicine 1 (1): 29. doi:10.1186/2001-1326-1-29.
- ^ Pritchard DI (2005). "Sourcing a chemical succession for cyclosporin from parasites and human pathogens". Drug Discovery Today 10 (10): 688–691. doi:10.1016/S1359-6446(05)03395-7. PMID 15896681.
- ^ McAlister VC, Mahalati K, Peltekian KM, Fraser A, MacDonald AS (June 2002). "A clinical pharmacokinetic study of tacrolimus and sirolimus combination immunosuppression comparing simultaneous to separated administration.". Ther Drug Monit. 24 (3): 346–50. doi:10.1097/00007691-200206000-00004. PMID 12021624.
- ^ "Cypher Sirolimus-eluting Coronary Stent". Cypher Stent. Retrieved 2008-04-01.
- ^ Shuchman M (2006). "Trading restenosis for thrombosis? New questions about drug-eluting stents". N Engl J Med 355 (19): 1949–52. doi:10.1056/NEJMp068234. PMID 17093244.
- ^ a b c d e f g "Rapamune Prescribing Information" (PDF). United States Food and Drug Administration. Wyeth Pharmaceuticals, Inc. May 2015. Retrieved 28 May 2016.
- ^ Lamming DW, Ye L, Katajisto P; Ye; Katajisto; Goncalves; Saitoh; Stevens; Davis; Salmon; Richardson; Ahima; Guertin; Sabatini; Baur; et al. (March 2012). "Rapamycin-induced insulin resistance is mediated by mTORC2 loss and uncoupled from longevity". Science 335 (6076): 1638–43. Bibcode:2012Sci...335.1638L. doi:10.1126/science.1215135. PMC 3324089. PMID 22461615.
- ^ Johnston, Olwyn; Rose, Caren L.; Webster, Angela C.; Gill, John S. (2008-07-01). "Sirolimus is associated with new-onset diabetes in kidney transplant recipients". Journal of the American Society of Nephrology: JASN 19 (7): 1411–1418. doi:10.1681/ASN.2007111202. ISSN 1533-3450. PMC 2440303. PMID 18385422.
- ^ Arriola Apelo, Sebastian I.; Neuman, Joshua C.; Baar, Emma L.; Syed, Faizan A.; Cummings, Nicole E.; Brar, Harpreet K.; Pumper, Cassidy P.; Kimple, Michelle E.; Lamming, Dudley W. (2015-10-13). "Alternative rapamycin treatment regimens mitigate the impact of rapamycin on glucose homeostasis and the immune system". Aging Cell. doi:10.1111/acel.12405. ISSN 1474-9726. PMID 26463117.
- ^ a b Chhajed PN, Dickenmann M, Bubendorf L, Mayr M, Steiger J, Tamm M (2006). "Patterns of pulmonary complications associated with sirolimus". Respiration 73 (3): 367–74. doi:10.1159/000087945. PMID 16127266.
- ^ Morelon E, Stern M, Israël-Biet D, et al. (September 2001). "Characteristics of sirolimus-associated interstitial pneumonitis in renal transplant patients". Transplantation 72 (5): 787–90. doi:10.1097/00007890-200109150-00008. PMID 11571438.
- ^ Filippone EJ, Carson JM, Beckford RA, et al. (September 2011). "Sirolimus-induced pneumonitis complicated by pentamidine-induced phospholipidosis in a renal transplant recipient: a case report". Transplant. Proc. 43 (7): 2792–7. doi:10.1016/j.transproceed.2011.06.060. PMID 21911165.
- ^ Pham PT, Pham PC, Danovitch GM, et al. (April 2004). "Sirolimus-associated pulmonary toxicity". Transplantation 77 (8): 1215–20. doi:10.1097/01.TP.0000118413.92211.B6. PMID 15114088.
- ^ Mingos MA, Kane GC (December 2005). "Sirolimus-induced interstitial pneumonitis in a renal transplant patient" (PDF). Respir Care 50 (12): 1659–61. PMID 16318648.
- ^ Das BB, Shoemaker L, Subramanian S, Johnsrude C, Recto M, Austin EH (March 2007). "Acute sirolimus pulmonary toxicity in an infant heart transplant recipient: case report and literature review". J. Heart Lung Transplant. 26 (3): 296–8. doi:10.1016/j.healun.2006.12.004. PMID 17346635.
- ^ Delgado JF, Torres J, José Ruiz-Cano M, et al. (September 2006). "Sirolimus-associated interstitial pneumonitis in 3 heart transplant recipients". J. Heart Lung Transplant. 25 (9): 1171–4. doi:10.1016/j.healun.2006.05.013. PMID 16962483.
- ^ McWilliams TJ, Levvey BJ, Russell PA, Milne DG, Snell GI (February 2003). "Interstitial pneumonitis associated with sirolimus: a dilemma for lung transplantation". J. Heart Lung Transplant. 22 (2): 210–3. doi:10.1016/S1053-2498(02)00564-8. PMID 12581772.
- ^ Aparicio G, Calvo MB, Medina V, et al. (August 2009). "Comprehensive lung injury pathology induced by mTOR inhibitors". Clin Transl Oncol 11 (8): 499–510. doi:10.1007/s12094-009-0394-y. PMID 19661024.
- ^ Paris A, Goupil F, Kernaonet E, et al. (January 2012). "[Drug-induced pneumonitis due to sirolimus: an interaction with atorvastatin?]". Rev Mal Respir (in French) 29 (1): 64–9. doi:10.1016/j.rmr.2010.03.026. PMID 22240222.
- ^ Maroto JP, Hudes G, Dutcher JP, et al. (May 2011). "Drug-related pneumonitis in patients with advanced renal cell carcinoma treated with temsirolimus". J. Clin. Oncol. 29 (13): 1750–6. doi:10.1200/JCO.2010.29.2235. PMID 21444868.
- ^ Errasti P, Izquierdo D, Martín P, et al. (October 2010). "Pneumonitis associated with mammalian target of rapamycin inhibitors in renal transplant recipients: a single-center experience". Transplant. Proc. 42 (8): 3053–4. doi:10.1016/j.transproceed.2010.07.066. PMID 20970608.
- ^ http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3275b824-3f82-4151-2ab2-0036a9ba0acc
- ^ a b c Schwecke T, Aparicio JF, Molnár I; Aparicio; Molnar; Konig; Khaw; Haycock; Oliynyk; Caffrey; Cortes; Lester; Bohm; Staunton; Leadlay; et al. (August 1995). "The biosynthetic gene cluster for the polyketide immunosuppressant rapamycin". Proc. Natl. Acad. Sci. U.S.A. 92 (17): 7839–43. Bibcode:1995PNAS...92.7839S. doi:10.1073/pnas.92.17.7839. PMC 41241. PMID 7644502.
- ^ Gregory MA, Gaisser S, Lill RE, et al. (May 2004). "Isolation and characterization of pre-rapamycin, the first macrocyclic intermediate in the biosynthesis of the immunosuppressant rapamycin by S. hygroscopicus". Angew. Chem. Int. Ed. Engl. 43 (19): 2551–3. doi:10.1002/anie.200453764. PMID 15127450.
- ^ Gregory MA, Hong H, Lill RE, et al. (October 2006). "Rapamycin biosynthesis: Elucidation of gene product function". Org. Biomol. Chem. 4 (19): 3565–8. doi:10.1039/b608813a. PMID 16990929.
- ^ Graziani EI (May 2009). "Recent advances in the chemistry, biosynthesis and pharmacology of rapamycin analogs". Nat Prod Rep 26 (5): 602–9. doi:10.1039/b804602f. PMID 19387497.
- ^ Gatto, G. J., Jr.; Boyne, M. T., II; Kelleher,N. L.; Walsh, C. T. (2006). "Biosynthesis of Pipecolic Acid by RapL, a Lysine Cyclodeaminase Encoded in the Rapamycin Gene Cluster". J. Am. Chem. Soc. 128 (11): 3838–47. doi:10.1021/ja0587603. PMID 16536560.
- ^ Aparicio JF, Molnár I, Schwecke T, et al. (February 1996). "Organization of the biosynthetic gene cluster for rapamycin in Streptomyces hygroscopicus: analysis of the enzymatic domains in the modular polyketide synthase". Gene 169 (1): 9–16. doi:10.1016/0378-1119(95)00800-4. PMID 8635756.
- ^ Li, Q; Rao, R; Vazzana, J; Goedegebuure, P; Odunsi, K; Gillanders, W; Shrikant, PA (2012). "Regulating mammalian target of rapamycin to tune vaccination-induced CD8(+) T cell responses for tumor immunity". Journal of immunology (Baltimore, Md. : 1950) 188 (7): 3080–7. doi:10.4049/jimmunol.1103365. PMC 3311730. PMID 22379028.
- ^ Easton, JB; Houghton, PJ (2006). "MTOR and cancer therapy". Oncogene 25 (48): 6436–46. doi:10.1038/sj.onc.1209886. PMID 17041628.
- ^ Law BK (October 2005). "Rapamycin: an anti-cancer immunosuppressant?". Crit. Rev. Oncol. Hematol. 56 (1): 47–60. doi:10.1016/j.critrevonc.2004.09.009. PMID 16039868.
- ^ Fatal AEs Higher with mTOR Drugs in Cancer. Med Page Today
- ^ Sun SY, Rosenberg LM, Wang X, et al. (August 2005). "Activation of Akt and eIF4E survival pathways by rapamycin-mediated mammalian target of rapamycin inhibition". Cancer Res. 65 (16): 7052–8. doi:10.1158/0008-5472.CAN-05-0917. PMID 16103051.
- ^ Chan S (2004). "Targeting the mammalian target of rapamycin (mTOR): a new approach to treating cancer". Br J Cancer 91 (8): 1420–4. doi:10.1038/sj.bjc.6602162. PMC 2409926. PMID 15365568.
- ^ Wendel HG, De Stanchina E, Fridman JS; Stanchina; Fridman; Malina; Ray; Kogan; Cordon-Cardo; Pelletier; Lowe; et al. (March 2004). "Survival signalling by Akt and eIF4E in oncogenesis and cancer therapy". Nature 428 (6980): 332–7. Bibcode:2004Natur.428..332W. doi:10.1038/nature02369. PMID 15029198. Lay summary – ScienceDaily (2004-03-18).
- ^ Novak, Kristine (May 2004). "Therapeutics: Means to an end". Nature Reviews Cancer 4 (5): 332. doi:10.1038/nrc1349.
- ^ Tuberous Sclerosis Alliance (October 2009). "Current Clinical Trials". Retrieved 2009-10-14.
- ^ Powers R.W.; Kaeberlein, M; Caldwell, SD; Kennedy, BK; Fields, S; et al. (15 January 2006). "Extension of chronological life span in yeast by decreased TOR pathway signaling". Genes & Development 20 (2): 174–184. doi:10.1101/gad.1381406. PMC 1356109. PMID 16418483.
- ^ Harrison DE, Strong R, Sharp ZD; Strong; Sharp; Nelson; Astle; Flurkey; Nadon; Wilkinson; Frenkel; Carter; Pahor; Javors; Fernandez; Miller; et al. (8 July 2009). "Rapamycin fed late in life extends lifespan in genetically heterogeneous mice". Nature 460 (7253): 392–5. Bibcode:2009Natur.460..392H. doi:10.1038/nature08221. PMC 2786175. PMID 19587680. Lay summary – The Times (2009-07-08).
- ^ Miller RA, Harrison DE, Astle CM, Baur JA, Boyd AR, de Cabo R, Fernandez E, Flurkey K, Javors MA, Nelson JF, Orihuela CJ, Pletcher S, Sharp ZD, Sinclair D, Starnes JW, Wilkinson JE, Nadon NL, Strong R (February 2011). "Rapamycin, but not resveratrol or simvastatin, extends life span of genetically heterogeneous mice". J. Gerontol. A Biol. Sci. Med. Sci. 66 (2): 191–201. doi:10.1093/gerona/glq178. PMC 3021372. PMID 20974732.
- ^ Ingram DK, Roth GS (Feb–Mar 2011). "Glycolytic inhibition as a strategy for developing calorie restriction mimetics". Experimental Gerontology 46 (2-3): 148–54. doi:10.1016/j.exger.2010.12.001. PMID 21167272. Retrieved 28 September 2013.
- ^ Tardif, S; Ross, C; Bergman, P; Fernandez, E; Javors, M; Salmon, A; Spross, J; Strong, R; Richardson, A (July 19, 2014). "Testing Efficacy of Administration of the Antiaging Drug Rapamycin in a Nonhuman Primate, the Common Marmoset". J Gerontol A Biol Sci Med Sci 70: 577–588. doi:10.1093/gerona/glu101. PMID 25038772.
- ^ Check Hayden, Erika (October 30, 2014). "Pet dogs set to test anti-ageing drug". Nature 514 (7524): 546. doi:10.1038/514546a. PMID 25355339. Retrieved 2 April 2015.
- ^ Amy Harmon (May 16, 2016). "Dogs Test Drug Aimed at Humans’ Biggest Killer: Age". The New York Times. Retrieved May 18, 2016.
- ^ Jagannath, Chinnaswamy; Bakhru, Pearl (2012). "Rapamycin-induced enhancement of vaccine efficacy in mice". Methods Mol Biol. Methods in Molecular Biology 821: 295–303. doi:10.1007/978-1-61779-430-8_18. ISBN 978-1-61779-429-2. PMID 22125073.
- ^ Mannick, JB; Del Giudice, G; Lattanzi, M; Valiante, NM; Paestgaard, J; Huang, B; Lonetto, MA; Maecker, HT; Kovarik, J; Carson, S; Klickstein, LB (December 24, 2014). "mTOR inhibition improves immune function in the elderly". Sci Transl Med 6 (268): 268ra179. doi:10.1126/scitranslmed.3009892. PMID 25540326.
- ^ Leontieva, Olga V.; Paszkiewicz, Geraldine M.; Blagosklonny, Mikhail V. (2014-01-01). "Comparison of rapamycin schedules in mice on high-fat diet". Cell Cycle (Georgetown, Tex.) 13 (21): 3350–3356. doi:10.4161/15384101.2014.970491. ISSN 1551-4005. PMC 4614913. PMID 25485580.
- ^ Leontieva, Olga V.; Paszkiewicz, Geraldine M.; Blagosklonny, Mikhail V. (2014-08-01). "Weekly administration of rapamycin improves survival and biomarkers in obese male mice on high-fat diet". Aging Cell 13 (4): 616–622. doi:10.1111/acel.12211. ISSN 1474-9726. PMC 4326934. PMID 24655348.
- ^ Popovich, Irina G.; Anisimov, Vladimir N.; Zabezhinski, Mark A.; Semenchenko, Anna V.; Tyndyk, Margarita L.; Yurova, Maria N.; Blagosklonny, Mikhail V. (2014-05-01). "Lifespan extension and cancer prevention in HER-2/neu transgenic mice treated with low intermittent doses of rapamycin". Cancer Biology & Therapy 15 (5): 586–592. doi:10.4161/cbt.28164. ISSN 1555-8576. PMC 4026081. PMID 24556924.
- ^ Arriola Apelo, Sebastian I.; Neuman, Joshua C.; Baar, Emma L.; Syed, Faizan A.; Cummings, Nicole E.; Brar, Harpreet K.; Pumper, Cassidy P.; Kimple, Michelle E.; Lamming, Dudley W. (2016-02-01). "Alternative rapamycin treatment regimens mitigate the impact of rapamycin on glucose homeostasis and the immune system". Aging Cell 15 (1): 28–38. doi:10.1111/acel.12405. ISSN 1474-9726. PMC 4717280. PMID 26463117.
- ^ Arriola Apelo, Sebastian I.; Pumper, Cassidy P.; Baar, Emma L.; Cummings, Nicole E.; Lamming, Dudley W. (2016-04-18). "Intermittent Administration of Rapamycin Extends the Life Span of Female C57BL/6J Mice". The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. doi:10.1093/gerona/glw064. ISSN 1758-535X. PMID 27091134.
- ^ Makki, Kassem; Taront, Solenne; Molendi-Coste, Olivier; Bouchaert, Emmanuel; Neve, Bernadette; Eury, Elodie; Lobbens, Stéphane; Labalette, Myriam; Duez, Hélène (2014-01-01). "Beneficial metabolic effects of rapamycin are associated with enhanced regulatory cells in diet-induced obese mice". PloS One 9 (4): e92684. doi:10.1371/journal.pone.0092684. ISSN 1932-6203. PMC 3977858. PMID 24710396.
- ^ Strong, Randy; Miller, Richard A.; Antebi, Adam; Astle, Clinton M.; Bogue, Molly; Denzel, Martin S.; Fernandez, Elizabeth; Flurkey, Kevin; Hamilton, Karyn L. (2016-06-16). "Longer lifespan in male mice treated with a weakly estrogenic agonist, an antioxidant, an α-glucosidase inhibitor or a Nrf2-inducer". Aging Cell. doi:10.1111/acel.12496. ISSN 1474-9726. PMID 27312235.
- ^ Jocelyn Rice (8 July 2009). "First Drug Shown to Extend Life Span in Mammals". Technology Review (Massachusetts Institute of Technology): 1–2. Retrieved 2009-07-09.
- ^ a b Powers RW, Kaeberlein M, Caldwell SD, Kennedy BK, Fields S (Jan 2006). "Extension of chronological life span in yeast by decreased TOR pathway signaling". Genes & Development 20 (2): 174–84. doi:10.1101/gad.1381406. PMC 1356109. PMID 16418483.
- ^ a b Kaeberlein M, Powers RW, Steffen KK, Westman EA, Hu D, Dang N, Kerr EO, Kirkland KT, Fields S, Kennedy BK (Nov 2005). "Regulation of yeast replicative life span by TOR and Sch9 in response to nutrients". Science 310 (5751): 1193–6. doi:10.1126/science.1115535. PMID 16293764.
- ^ Jia K, Chen D, Riddle DL (Aug 2004). "The TOR pathway interacts with the insulin signaling pathway to regulate C. elegans larval development, metabolism and life span". Development 131 (16): 3897–906. doi:10.1242/dev.01255. PMID 15253933.
- ^ Kapahi P, Zid BM, Harper T, Koslover D, Sapin V, Benzer S (May 2004). "Regulation of lifespan in Drosophila by modulation of genes in the TOR signaling pathway". Current Biology 14 (10): 885–90. doi:10.1016/j.cub.2004.03.059. PMC 2754830. PMID 15186745.
- ^ Harrison DE, Strong R, Sharp ZD, Nelson JF, Astle CM, Flurkey K, Nadon NL, Wilkinson JE, Frenkel K, Carter CS, Pahor M, Javors MA, Fernandez E, Miller RA (Jul 2009). "Rapamycin fed late in life extends lifespan in genetically heterogeneous mice". Nature 460 (7253): 392–5. doi:10.1038/nature08221. PMC 2786175. PMID 19587680.
- ^ Miller RA, Harrison DE, Astle CM, Fernandez E, Flurkey K, Han M, Javors MA, Li X, Nadon NL, Nelson JF, Pletcher S, Salmon AB, Sharp ZD, Van Roekel S, Winkleman L, Strong R (Jun 2014). "Rapamycin-mediated lifespan increase in mice is dose and sex dependent and metabolically distinct from dietary restriction". Aging Cell 13 (3): 468–77. doi:10.1111/acel.12194. PMC 4032600. PMID 24341993.
- ^ Fok WC, Chen Y, Bokov A, Zhang Y, Salmon AB, Diaz V, Javors M, Wood WH, Zhang Y, Becker KG, Pérez VI, Richardson A (2014-01-01). "Mice fed rapamycin have an increase in lifespan associated with major changes in the liver transcriptome". PLOS ONE 9 (1): e83988. doi:10.1371/journal.pone.0083988. PMC 3883653. PMID 24409289.
- ^ Cota D, Proulx K, Smith KA, Kozma SC, Thomas G, Woods SC, Seeley RJ (2006). "Hypothalamic mTOR signaling regulates food intake". Science 312 (5775): 927–930. doi:10.1126/science.1124147. PMID 16690869.
- ^ a b Kriete A, Bosl WJ, Booker G (June 2010). "Rule-Based Cell Systems Model of Aging using Feedback Loop Motifs Mediated by Stress Responses". PLoS Computational Biology 6 (6): e1000820. doi:10.1371/journal.pcbi.1000820. PMC 2887462. PMID 20585546.
- ^ Magnuson, Brian; Ekim, Bilgen; Fingar, Diane C. (2012-01-01). "Regulation and function of ribosomal protein S6 kinase (S6K) within mTOR signalling networks". The Biochemical Journal 441 (1): 1–21. doi:10.1042/BJ20110892. ISSN 1470-8728. PMID 22168436.
- ^ a b Schieke SM, Phillips D, McCoy JP, Aponte AM, Shen RF, Balaban RS, Finkel T (2006). "The Mammalian Target of Rapamycin (mTOR) Pathway Regulates Mitochondrial Oxygen Consumption and Oxidative Capacity". J. Biol. Chem. 281 (37): 27643–27652. doi:10.1074/jbc.M603536200. PMID 16847060.
- ^ Ehninger D, Han S, Shilyansky C, et al. "Reversal of learning deficits in a Tsc2+/- mouse model of tuberous sclerosis". Nat. Med. 14 (8): 843–8. doi:10.1038/nm1788. PMC 2664098. PMID 18568033.
- ^ ScienceDaily.com Report
- ^ Spilman P, Podlutskaya N, Hart MJ, et al. (2010). Ferrari PF, ed. "Inhibition of mTOR by rapamycin abolishes cognitive deficits and reduces amyloid-beta levels in a mouse model of Alzheimer's disease". PLoS ONE 5 (4): e9979. doi:10.1371/journal.pone.0009979. PMC 2848616. PMID 20376313.
- ^ "Nanoparticles treat muscular dystrophy in mice | Newsroom | Washington University in St. Louis". News.wustl.edu. Retrieved 2014-04-07.
- ^ Fernandez, D; Bonilla, E; Mirza, N; Niland, B; Perl, A (2006). "Rapamycin reduces disease activity and normalizes T cell activation-induced calcium fluxing in patients with systemic lupus erythematosus". Arthritis & Rheumatism 54 (9): 2983–8. doi:10.1002/art.22085. PMC 4034146. PMID 16947529.
- ^ Fernandez, D. R.; Telarico, T; Bonilla, E; Li, Q; Banerjee, S; Middleton, F. A.; Phillips, P. E.; Crow, M. K.; Oess, S; Muller-Esterl, W; Perl, A (2009). "Activation of mammalian target of rapamycin controls the loss of TCRzeta in lupus T cells through HRES-1/Rab4-regulated lysosomal degradation". The Journal of Immunology 182 (4): 2063–73. doi:10.4049/jimmunol.0803600. PMC 2676112. PMID 19201859.
- ^ Fernandez, D; Perl, A (2010). "MTOR signaling: A central pathway to pathogenesis in systemic lupus erythematosus?". Discovery medicine 9 (46): 173–8. PMC 3131182. PMID 20350481.
- ^ Lai, Z. W.; Borsuk, R; Shadakshari, A; Yu, J; Dawood, M; Garcia, R; Francis, L; Tily, H; Bartos, A; Faraone, S. V.; Phillips, P; Perl, A (2013). "Mechanistic target of rapamycin activation triggers IL-4 production and necrotic death of double-negative T cells in patients with systemic lupus erythematosus". The Journal of Immunology 191 (5): 2236–46. doi:10.4049/jimmunol.1301005. PMC 3777662. PMID 23913957.
- ^ Kato, H; Perl, A (2014). "Mechanistic Target of Rapamycin Complex 1 Expands Th17 and IL-4+ CD4-CD8- Double-Negative T Cells and Contracts Regulatory T Cells in Systemic Lupus Erythematosus". The Journal of Immunology 192 (9): 4134–44. doi:10.4049/jimmunol.1301859. PMC 3995867. PMID 24683191.
- ^ Caza, T. N.; Fernandez, D. R.; Talaber, G; Oaks, Z; Haas, M; Madaio, M. P.; Lai, Z. W.; Miklossy, G; Singh, R. R.; Chudakov, D. M.; Malorni, W; Middleton, F; Banki, K; Perl, A (2013). "HRES-1/Rab4-mediated depletion of Drp1 impairs mitochondrial homeostasis and represents a target for treatment in SLE". Annals of the Rheumatic Diseases 73: 1888–1897. doi:10.1136/annrheumdis-2013-203794. PMID 23897774.
- ^ Donia M, McCubrey JA, Bendtzen K, Nicoletti F (December 2010). "Potential use of rapamycin in HIV infection". Br J Clin Pharmacol 70 (6): 784–93. doi:10.1111/j.1365-2125.2010.03735.x. PMC 3014061. PMID 21175433.
- ^ Campbell GR, Spector SA (March 2011). "Hormonally active vitamin D3 (1{alpha},25-dihydroxycholecalciferol) triggers autophagy in human macrophages that inhibits HIV-1 infection". J Biol Chem 286 (21): 18890–902. doi:10.1074/jbc.M110.206110. PMID 21454634.
- ^ Peces R, Peces C, Pérez-Dueñas V, et al. (16 January 2009). "Rapamycin reduces kidney volume and delays the loss of renal function in a patient with autosomal-dominant polycystic kidney disease". NDT Plus (Oxford Journals) 2 (2): 133–5. doi:10.1093/ndtplus/sfn210. ISSN 1753-0792.
- ^ CNN.com Clue to kids' early aging disease found, July 1, 2011
- ^ Rivera, VM; Clackson, T; Natesan, S; Pollock, R; Amara, JF; Keenan, T; Magari, SR; Phillips, T; Courage, NL; Cerasoli F, Jr; Holt, DA; Gilman, M (September 1996). "A humanized system for pharmacologic control of gene expression". Nature Medicine 2 (9): 1028–32. doi:10.1038/nm0996-1028. PMID 8782462.
External links[edit]
| Wikimedia Commons has media related to Sirolimus. |



