- published: 12 Jan 2010
- views: 13971
-
remove the playlistFilm Treatment
- remove the playlistFilm Treatment
- published: 20 Nov 2015
- views: 153415
- published: 24 Oct 2013
- views: 249960
- published: 19 Feb 2014
- views: 33956
- published: 03 Jul 2014
- views: 30118
Film treatment
A film treatment (or simply treatment) is a piece of prose, typically the step between scene cards (index cards) and the first draft of a screenplay for a motion picture, television program, or radio play. It is generally longer and more detailed than an outline (or one-page synopsis), and it may include details of directorial style that an outline omits. Treatments read like a short story, but are told in the present tense and describe events as they happen.
Original draft treatment
The original draft treatment is created during the writing process, and is generally long and detailed. It consists of full-scene outlines put together. Usually there are between thirty to eighty standard letter size or A4 pages (Courier New 12 point), with an average of about forty pages. For example, The Terminator is forty-eight pages.
More elaborate forms of the draft treatment are the step outline and the scriptment.
Presentation treatment
The presentation treatment is created as presentation material. Generally the scene card descriptions are written out in order, and only have the essential and important story events that make up the scenes. It is the full story in its simplest form, moving from the concept, to the theme, to the character, to the detailed synopsis of about four to eight pages of master scenes.
This article is licensed under the Creative Commons Attribution-ShareAlike 3.0 Unported License, which means that you can copy and modify it as long as the entire work (including additions) remains under this license.
- Loading...

-
 5:13
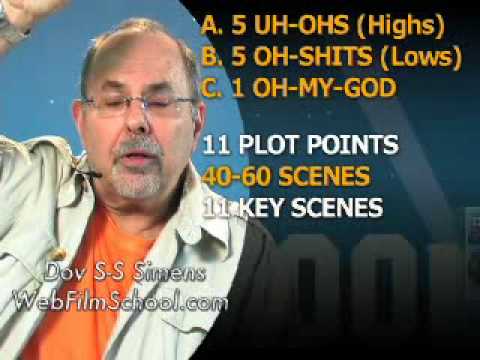
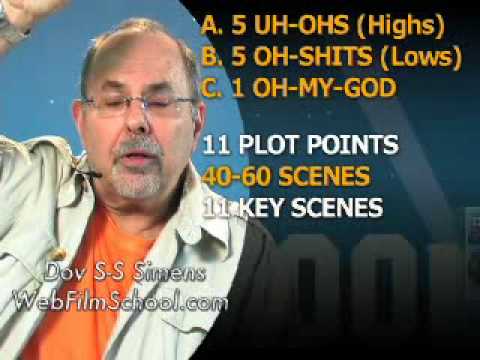
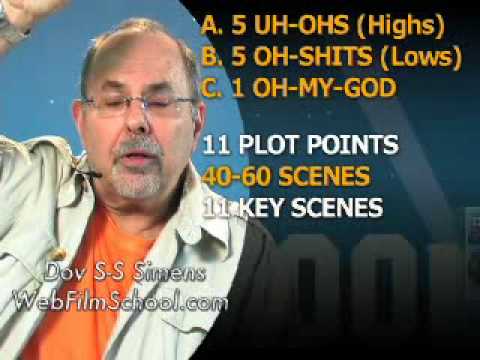
5:13Screenplay Treatment (Web Film School 33)
Screenplay Treatment (Web Film School 33) -
 3:02
3:02Writing A Film Treatment
Writing A Film TreatmentWriting A Film Treatment
http://screenwritersforhire.com -
 15:15
15:15Love Treatment || Latest Telugu Short Film 2015 || Directed By Sravan Jadala
Love Treatment || Latest Telugu Short Film 2015 || Directed By Sravan JadalaLove Treatment || Latest Telugu Short Film 2015 || Directed By Sravan Jadala
Love Treatment is Latest Telugu Short Film 2015 presented By Runwayreel Casting Harish Suman Rudru Jahnavi Dasetty Arjun Chelluri Gayathri Archak Divya Surthi Baby JaiSree Crishna Nandyala SreeHari Rudreshwar Reddy Sreekanth Reddy Sravan Jadala Dop : Nikhil Ronald Asst Dop : Bhaanu Chander golluri Posters : Madhu macherla Vishnu Vardhan Reddy Asst Directors : Priyanka Ij Crishna Nandyala (Nandhu) Music : Rohit Jilla Titles : Srinivas Di : Ratnakar Reddy Indra karna Goud Producers : Suryam Babu Jadala Sreekanth Reddy k Concept, Screenplay, Editing & Director Sravan Jadala Subscribe for more Entertainment: http://goo.gl/gEhKD Like us on FB @ https://www.facebook.com/RunwayReel Follow us on Twitter @ https://twitter.com/RunwayReel Latest Telugu Short Films 2015 : http://goo.gl/jAOTMe Latest Telugu Short film 2013 : http://goo.gl/yEM52r Latest telugu Short film 2014 : http://goo.gl/F62FPr Telugu Latest Video Songs : http://goo.gl/pGtxUC -
 2:04
2:04The Treatment International Trailer
The Treatment International TrailerThe Treatment International Trailer
Inspector Nick Cafmeyer seems to have it all : the looks, the brains, the career outlook. Yet a dark shadow is hanging over his life and relationships. Since age 9, Nick has been haunted by the unsolved disappearance of his younger brother Bjorn. Based on Nick's testimony, their neighbour, Plettinckx, a known sex offender, was questioned but soon released. After all these years, Plettinckx still lives closeby and takes fiendish pleasure in harassing Nick. The only woman able to sustain an on-off relationship with Nick, is his chief, Danni, who is slightly older. She is reluctant to involve Nick in a very disturbing case: a couple has been held captive for three days by an intruder. The intruder has vanished without a trace, along with their 9-year old son Robin. Nick heads a massive search and turns it into a relentless manhunt. -
 5:49
5:49Treatment (a Marathi Comedy Short Film)
Treatment (a Marathi Comedy Short Film) -
 7:38
7:38Treatment HD Marathi Funny Short Film
Treatment HD Marathi Funny Short Film -
 13:08
13:08Disturbing Film: Symptoms of Schizophrenia - Medicine, Psychiatry, Patients & Treatment (1940s)
Disturbing Film: Symptoms of Schizophrenia - Medicine, Psychiatry, Patients & Treatment (1940s)Disturbing Film: Symptoms of Schizophrenia - Medicine, Psychiatry, Patients & Treatment (1940s)
In the early 20th century, the psychiatrist Kurt Schneider listed the forms of psychotic symptoms that he thought distinguished schizophrenia from other psychotic disorders. These are called first-rank symptoms or Schneider's first-rank symptoms. They include delusions of being controlled by an external force; the belief that thoughts are being inserted into or withdrawn from one's conscious mind; the belief that one's thoughts are being broadcast to other people; and hearing hallucinatory voices that comment on one's thoughts or actions or that have a conversation with other hallucinated voices. Although they have significantly contributed to the current diagnostic criteria, the specificity of first-rank symptoms has been questioned. A review of the diagnostic studies conducted between 1970 and 2005 found that they allow neither a reconfirmation nor a rejection of Schneider's claims, and suggested that first-rank symptoms should be de-emphasized in future revisions of diagnostic systems. The history of schizophrenia is complex and does not lend itself easily to a linear narrative. Accounts of a schizophrenia-like syndrome are thought to be rare in historical records before the 19th century, although reports of irrational, unintelligible, or uncontrolled behavior were common. A detailed case report in 1797 concerning James Tilly Matthews, and accounts by Phillipe Pinel published in 1809, are often regarded as the earliest cases of the illness in the medical and psychiatric literature. The Latinized term dementia praecox was first used by German alienist Heinrich Schule in 1886 and then in 1891 by Arnold Pick in a case report of a psychotic disorder (hebephrenia). In 1893 Emil Kraepelin borrowed the term from Schule and Pick and in 1899 introduced a broad new distinction in the classification of mental disorders between dementia praecox and mood disorder (termed manic depression and including both unipolar and bipolar depression). Kraepelin believed that dementia praecox was probably caused by a long-term, smouldering systemic or "whole body" disease process that affected many organs and peripheral nerves in the body but which affected the brain after puberty in a final decisive cascade. His use of the term dementia distinguished it from other forms of dementia such as Alzheimer's disease which typically occur later in life. It is sometimes argued that the use of the term démence précoce in 1852 by the French physician Bénédict Morel constitutes the medical discovery of schizophrenia. However this account ignores the fact that there is little to connect Morel's descriptive use of the term and the independent development of the dementia praecox disease concept at the end of the nineteenth-century. The word schizophrenia—which translates roughly as "splitting of the mind" and comes from the Greek roots schizein (σχίζειν, "to split") and phrēn, phren- (φρήν, φρεν-, "mind")—was coined by Eugen Bleuler in 1908 and was intended to describe the separation of function between personality, thinking, memory, and perception. American and British interpretations of Beuler led to the claim that he described its main symptoms as 4 A's: flattened Affect, Autism, impaired Association of ideas and Ambivalence. Bleuler realized that the illness was not a dementia, as some of his patients improved rather than deteriorated, and thus proposed the term schizophrenia instead. Treatment was revolutionized in the mid-1950s with the development and introduction of chlorpromazine. In the early 1970s, the diagnostic criteria for schizophrenia were the subject of a number of controversies which eventually led to the operational criteria used today. It became clear after the 1971 US-UK Diagnostic Study that schizophrenia was diagnosed to a far greater extent in America than in Europe. This was partly due to looser diagnostic criteria in the US, which used the DSM-II manual, contrasting with Europe and its ICD-9. David Rosenhan's 1972 study, published in the journal Science under the title "On being sane in insane places", concluded that the diagnosis of schizophrenia in the US was often subjective and unreliable. These were some of the factors leading to the revision not only of the diagnosis of schizophrenia, but the revision of the whole DSM manual, resulting in the publication of the DSM-III in 1980. The term schizophrenia is commonly misunderstood to mean that affected persons have a "split personality". Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct multiple personalities. http://en.wikipedia.org/wiki/Schizophrenia -
 100:23
100:23刮痧 The Gua Sha Treatment
刮痧 The Gua Sha Treatment刮痧 The Gua Sha Treatment
The Gua Sha Treatment (Chinese: 刮痧; pinyin: guā shā) is a Chinese movie released in 2001 starring Tony Leung Ka-Fai, Zhu Xu, and Jiang Wenli. It is a story about cultural conflicts experienced by a Chinese family in the USA. -
 4:54
4:54Screenplay Treatment II (Web Film School 34)
Screenplay Treatment II (Web Film School 34) -
 0:48
0:48Silent Treatment - Short Film: Teaser Trailer
Silent Treatment - Short Film: Teaser Trailer
-

-

Writing A Film Treatment
http://screenwritersforhire.com -

Love Treatment || Latest Telugu Short Film 2015 || Directed By Sravan Jadala
Love Treatment is Latest Telugu Short Film 2015 presented By Runwayreel Casting Harish Suman Rudru Jahnavi Dasetty Arjun Chelluri Gayathri Archak Divya Surthi Baby JaiSree Crishna Nandyala SreeHari Rudreshwar Reddy Sreekanth Reddy Sravan Jadala Dop : Nikhil Ronald Asst Dop : Bhaanu Chander golluri Posters : Madhu macherla Vishnu Vardhan Reddy Asst Directors : Priyanka Ij Crishna Nandyala (Nandhu) Music : Rohit Jilla Titles : Srinivas Di : Ratnakar Reddy Indra karna Goud Producers : Suryam Babu Jadala Sreekanth Reddy k Concept, Screenplay, Editing & Director Sravan Jadala Subscribe for more Entertainment: http://goo.gl/gEhKD Like us ... -

The Treatment International Trailer
Inspector Nick Cafmeyer seems to have it all : the looks, the brains, the career outlook. Yet a dark shadow is hanging over his life and relationships. Since age 9, Nick has been haunted by the unsolved disappearance of his younger brother Bjorn. Based on Nick's testimony, their neighbour, Plettinckx, a known sex offender, was questioned but soon released. After all these years, Plettinckx still lives closeby and takes fiendish pleasure in harassing Nick. The only woman able to sustain an on-off relationship with Nick, is his chief, Danni, who is slightly older. She is reluctant to involve Nick in a very disturbing case: a couple has been held captive for three days by an intruder. The intruder has vanished without a trace, along with their 9-year old son Robin. Nick heads a massive search... -

-

-

Disturbing Film: Symptoms of Schizophrenia - Medicine, Psychiatry, Patients & Treatment (1940s)
In the early 20th century, the psychiatrist Kurt Schneider listed the forms of psychotic symptoms that he thought distinguished schizophrenia from other psychotic disorders. These are called first-rank symptoms or Schneider's first-rank symptoms. They include delusions of being controlled by an external force; the belief that thoughts are being inserted into or withdrawn from one's conscious mind; the belief that one's thoughts are being broadcast to other people; and hearing hallucinatory voices that comment on one's thoughts or actions or that have a conversation with other hallucinated voices. Although they have significantly contributed to the current diagnostic criteria, the specificity of first-rank symptoms has been questioned. A review of the diagnostic studies conducted between 19... -

刮痧 The Gua Sha Treatment
The Gua Sha Treatment (Chinese: 刮痧; pinyin: guā shā) is a Chinese movie released in 2001 starring Tony Leung Ka-Fai, Zhu Xu, and Jiang Wenli. It is a story about cultural conflicts experienced by a Chinese family in the USA. -
-

Screenplay Treatment (Web Film School 33)
- Order: Reorder
- Duration: 5:13
- Updated: 12 Jan 2010
- views: 13971
Writing A Film Treatment
- Order: Reorder
- Duration: 3:02
- Updated: 16 Aug 2012
- views: 351
Love Treatment || Latest Telugu Short Film 2015 || Directed By Sravan Jadala
- Order: Reorder
- Duration: 15:15
- Updated: 20 Nov 2015
- views: 153415
- published: 20 Nov 2015
- views: 153415
The Treatment International Trailer
- Order: Reorder
- Duration: 2:04
- Updated: 24 Oct 2013
- views: 249960
- published: 24 Oct 2013
- views: 249960
Treatment (a Marathi Comedy Short Film)
- Order: Reorder
- Duration: 5:49
- Updated: 21 Jul 2012
- views: 107488
Treatment HD Marathi Funny Short Film
- Order: Reorder
- Duration: 7:38
- Updated: 31 Aug 2015
- views: 1945
Disturbing Film: Symptoms of Schizophrenia - Medicine, Psychiatry, Patients & Treatment (1940s)
- Order: Reorder
- Duration: 13:08
- Updated: 19 Feb 2014
- views: 33956
- published: 19 Feb 2014
- views: 33956
刮痧 The Gua Sha Treatment
- Order: Reorder
- Duration: 100:23
- Updated: 03 Jul 2014
- views: 30118
- published: 03 Jul 2014
- views: 30118
Screenplay Treatment II (Web Film School 34)
- Order: Reorder
- Duration: 4:54
- Updated: 12 Jan 2010
- views: 4908
Silent Treatment - Short Film: Teaser Trailer
- Order: Reorder
- Duration: 0:48
- Updated: 27 Jun 2013
- views: 2842
- Playlist
- Chat
- Playlist
- Chat

Screenplay Treatment (Web Film School 33)
- Report rights infringement
- published: 12 Jan 2010
- views: 13971

Writing A Film Treatment
- Report rights infringement
- published: 16 Aug 2012
- views: 351

Love Treatment || Latest Telugu Short Film 2015 || Directed By Sravan Jadala
- Report rights infringement
- published: 20 Nov 2015
- views: 153415

The Treatment International Trailer
- Report rights infringement
- published: 24 Oct 2013
- views: 249960

Treatment (a Marathi Comedy Short Film)
- Report rights infringement
- published: 21 Jul 2012
- views: 107488

Treatment HD Marathi Funny Short Film
- Report rights infringement
- published: 31 Aug 2015
- views: 1945

Disturbing Film: Symptoms of Schizophrenia - Medicine, Psychiatry, Patients & Treatment (1940s)
- Report rights infringement
- published: 19 Feb 2014
- views: 33956

刮痧 The Gua Sha Treatment
- Report rights infringement
- published: 03 Jul 2014
- views: 30118
Screenplay Treatment II (Web Film School 34)
- Report rights infringement
- published: 12 Jan 2010
- views: 4908

Silent Treatment - Short Film: Teaser Trailer
- Report rights infringement
- published: 27 Jun 2013
- views: 2842
iPhone 8 Leaks, New iPhone 7 Features Reported
Edit Inquisitr 09 Jul 2016Pakistan's 'Angel of Mercy' Edhi Dies at 88
Edit WorldNews.com 08 Jul 2016Wimbledon 2016: Serena Williams beats Angelique Kerber to win 22nd Grand Slam
Edit BBC News 09 Jul 2016Dallas shooting: Newlywed, Iraq veteran among police officers killed
Edit Deccan Chronicle 09 Jul 2016'He Had Many More Films To Make': Remembering Iranian Director Abbas Kiarostami
Edit National Public Radio 09 Jul 2016China launches drive to eradicate violence against hospital staff
Edit Indian Express 09 Jul 2016Film review: The Neon Demon | Maggie’s Plan | Ice Age: Collision Course
Edit Scotsman 09 Jul 2016Thousands rally across US cities to protest police brutality
Edit Press TV 09 Jul 2016A regime in denial
Edit Deccan Herald 09 Jul 2016Robert G. Montgomery commentary: Court must balance due process with treatment
Edit The Columbus Dispatch 09 Jul 2016It's confirmed! Deepika Padukone will star in 'Padmavati'
Edit The Times of India 09 Jul 2016Parvin Dabas: UP’s film policy can help the state promote its culture
Edit The Times of India 09 Jul 2016Bajura women live with health problems for years due to poverty
Edit The Himalayan 09 Jul 2016Harry Potter stuntman to play Ashwin’s villain
Edit The Times of India 09 Jul 2016Strides to stardom
Edit Deccan Herald 09 Jul 2016Has Rakul Preet Singh replaced Parineeti Chopra in the Mahesh Babu film?
Edit DNA India 09 Jul 2016I’m very critical about my work: Jimmy Sheirgill
Edit Indian Express 09 Jul 2016- 1
- 2
- 3
- 4
- 5
- Next page »







