- Order:
- Duration: 3:11
- Published: 27 Dec 2008
- Uploaded: 05 Aug 2011
- Author: JimLitzFilms






































| Diseasesdb | 33846 |
|---|---|
| Icd10 | |
| Icd9 | |
| Medlineplus | 000925 |
| Emedicinesubj | med |
| Emedicinetopic | 1900 |
| Meshid | D013313 |
Posttraumatic stress disorder (also known as post-traumatic stress disorder or PTSD) is a severe anxiety disorder that can develop after exposure to any event that results in psychological trauma. It has three sub-forms: acute, chronic, and delayed-onset.
Traumatic events that may cause PTSD symptoms to develop include violent assault, kidnapping, sexual assault, torture, being a hostage, prisoner of war or concentration camp victim, experiencing a disaster, violent automobile accidents or getting a diagnosis of a life-threatening illness. Preliminary research suggests that child abuse may interact with mutations in a stress-related gene to increase the risk of PTSD in adults.
Multiple studies show that parental PTSD and other posttraumatic disturbances in parental psychological functioning can, despite a traumatized parent's best efforts, interfere with their response to their child as well as their child's response to trauma. Parents with violence-related PTSD may, for example, inadvertently expose their children to developmentally inappropriate violent media due to their need to manage their own emotional dysregulation. Clinical findings indicate that a failure to provide adequate treatment to children after they suffer a traumatic experience, depending on their vulnerability and the severity of the trauma, will ultimately lead to PTSD symptoms in adulthood.
PTSD displays biochemical changes in the brain and body that differ from other psychiatric disorders such as major depression. Individuals diagnosed with PTSD respond more strongly to a dexamethasone suppression test than individuals diagnosed with clinical depression.
In addition, most people with PTSD also show a low secretion of cortisol and high secretion of catecholamines in urine, with a norepinephrine/cortisol ratio consequently higher than comparable non-diagnosed individuals. This is in contrast to the normative fight-or-flight response, in which both catecholamine and cortisol levels are elevated after exposure to a stressor.
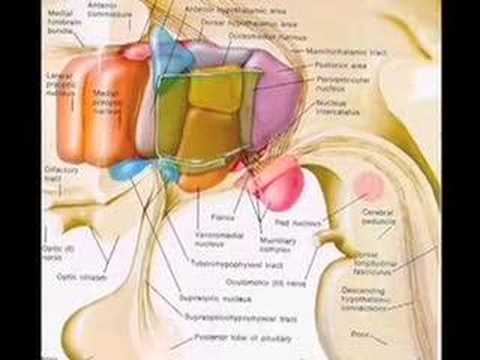
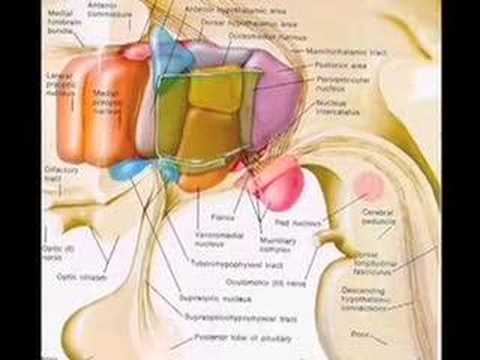
Brain catecholamine levels are low, and corticotropin-releasing factor (CRF) concentrations are high. Together, these findings suggest abnormality in the hypothalamic-pituitary-adrenal (HPA) axis.
Given the strong cortisol suppression to dexamethasone in PTSD, HPA axis abnormalities are likely predicated on strong negative feedback inhibition of cortisol, itself likely due to an increased sensitivity of glucocorticoid receptors. Some researchers have associated the response to stress in PTSD with long-term exposure to high levels of norepinephrine and low levels of cortisol, a pattern associated with improved learning in animals.
Translating this reaction to human conditions gives a pathophysiological explanation for PTSD by a maladaptive learning pathway to fear response through a hypersensitive, hyperreactive and hyperresponsive HPA axis.
Low cortisol levels may predispose individuals to PTSD: Following war trauma, Swedish soldiers serving in Bosnia and Herzegovina with low pre-service salivary cortisol levels had a higher risk of reacting with PTSD symptoms, following war trauma, than soldiers with normal pre-service levels. Because cortisol is normally important in restoring homeostasis after the stress response, it is thought that trauma survivors with low cortisol experience a poorly contained—that is, longer and more distressing—response, setting the stage for PTSD.
However, there is considerable controversy within the medical community regarding the neurobiology of PTSD. A review of existing studies on this subject showed no clear relationship between cortisol levels and PTSD. Only a slight majority have found a decrease in cortisol levels while others have found no effect or even an increase.
In human studies, the amygdala has been shown to be strongly involved in the formation of emotional memories, especially fear-related memories. Neuroimaging studies in humans have revealed both morphological and functional aspects of PTSD.
The amygdalocentric model of PTSD proposes that it is associated with hyperarousal of the amygdala and insufficient top-down control by the medial prefrontal cortex and the hippocampus particularly during extinction. This is consistent with an interpretation of PTSD as a syndrome of deficient extinction ability. Further animal and clinical research into the amygdala and fear conditioning may suggest additional treatments for the condition.
Recently, it has been found that several single-nucleotide polymorphisms (SNPs) in FK506 binding protein 5 (FKBP5) interact with childhood trauma to predict severity of adult PTSD. These findings suggest that individuals with these SNPs who are abused as children are more susceptible to PTSD as adults.
This is particularly interesting given that FKBP5 SNPs have previously been associated with peritraumatic dissociation (that is, dissociation at the time of the trauma), which has itself been shown to be predictive of PTSD. Furthermore, FKBP5 may be less expressed in those with current PTSD. Another recent study found a single SNP in a putative estrogen response element on ADCYAP1R1 (encodes pituitary adenylate cyclase-activating polypeptide type I receptor or PAC1) to predict PTSD diagnosis and symptoms in females. Incidentally, this SNP is also associated with fear discrimination. The study suggests that perturbations in the PACAP-PAC1 pathway are involved in abnormal stress responses underlying PTSD.
Although most people (50-90%) encounter trauma over a lifetime, only about 8% develop full PTSD. This effect of childhood trauma, which is not well understood, may be a marker for both traumatic experiences and attachment problems. Proximity to, duration of, and severity of the trauma also make an impact; and interpersonal traumas cause more problems than impersonal ones.
In one study (Dubner and Motta, 1999), 60% of children in foster care who had experienced sexual abuse had PTSD, and 42% of those who had been physically abused fulfilled the PTSD criteria. PTSD was also found in 18% of the children who were not abused. These children may have developed PTSD due to witnessing violence in the home, or as a result of real or perceived parental abandonment.
"Developmental trauma disorder", a proposed new diagnosis, was still under discussion at the time of the draft publication.
In recent history, catastrophes (by human means or not) such as the 2004 Indian Ocean tsunami may have caused PTSD in many survivors and rescue workers. Today relief workers from organizations such as the Red Cross and the Salvation Army provide counseling after major disasters as part of their standard procedures to curb severe cases of posttraumatic stress disorder.
A review of the provision of compensation to veterans for PTSD by the United States Department of Veterans Affairs began in 2005 after the VA had noted a 30% increase in PTSD claims in recent years. This led to a backlash from veterans'-rights groups, and to some highly publicized suicides by veterans who feared losing their benefits, which in some cases constituted their only income. In response, on November 10, 2005, the Secretary of Veterans Affairs announced that "the Department of Veterans Affairs (VA) will not review the files of 72,000 veterans currently receiving disability compensation for posttraumatic stress disorder..."
The diagnosis of PTSD in U.S. military veterans has been a subject of some controversy due to uncertainties in objectively diagnosing PTSD in those who may have been exposed to trauma, and due to this diagnosis' association with some incidence of compensation-seeking behavior.
Many veterans of the wars in Iraq and Afghanistan returning home have faced significant physical, emotional and relational disruptions. In response, the United States Marine Corps has instituted programs to assist them in re-adjusting to civilian life, especially in their relationships with spouses and loved ones, to help them communicate better and understand what the other has gone through. Walter Reed Army Institute of Research (WRAIR) developed the Battlemind program to assist service members avoid or ameliorate PTSD and related problems.
Veterans Affairs Canada offers a new program that includes rehabilitation, financial benefits, job placement, health benefits program, disability awards and family support.
Delhanty for example were able to identify that the forensic exam given to victims after a rape was associated with PTSD. Finally, global treatments attempt to avoid the problems of early detection by simply treating everyone involved. However, many studies
The psychotherapy programs with the strongest demonstrated efficacy include cognitive behavioral programs, variants of exposure therapy, stress inoculation training (SIT), variants of cognitive therapy (CT), eye movement desensitization and reprocessing (EMDR), and many combinations of these procedures. A 2010 review disagrees that these treatments have proven efficacy, and points out methodological flaws in the studies and previous meta-analyses.
EMDR or trauma-focused cognitive behavioral therapy (TFCBT) was recommended as first-line treatments for trauma victims in a 2007 review; however, "the evidence base [for EMDR] was not as strong as that for TFCBT ... Furthermore, there was limited evidence that TFCBT and EMDR were superior to supportive/non-directive treatments, hence it is highly unlikely that their effectiveness is due to non-specific factors such as attention." A meta-analytic comparison of EMDR and cognitive behavioral therapy found both protocols indistinguishable in terms of effectiveness in treating PTSD; however "the contribution of the eye movement component in EMDR to treatment outcome" is unclear.
Recent research on contextually based third-generation behavior therapies suggests that they may produce results comparable to some of the better validated therapies. Many of these therapy methods have a significant element of exposure, and have demonstrated success in treating the primary problems of PTSD and co-occurring depressive symptoms.
Exposure therapy is a type of cognitive behavioral therapy that involves assisting trauma survivors to re-experience distressing trauma-related memories and reminders in order to facilitate habituation and successful emotional processing of the trauma memory. Most exposure therapy programs include both imaginal confrontation with the traumatic memories and real-life exposure to trauma reminders; this therapy modality is well supported by clinical evidence. Indeed, the success of exposure-based therapies has raised the question of whether exposure is a necessary ingredient in the treatment of PTSD. Some organizations have endorsed the need for exposure. The US Department of Veterans Affairs has been actively training mental health treatment staff in Prolonged Exposure Therapy and Cognitive Processing Therapy in an effort to better treat US Veterans with PTSD.
Among the anti-depressants described in this section, bupropion and venlafaxine have the lowest patient drop-out rates. Sertraline, fluoxetine, and nefazodone have a modestly higher drop-out rate (~15%), and the heterocyclics and paroxetine have the highest rates (~20%+). Where drop-out is caused or feared because of medication side-effects, it should be remembered that most patients do not experience such side-effects.
Alpha-adrenergic antagonists. Prazosin ("Minipress"), in a small study of combat veterans, has shown substantial benefit in relieving or reducing nightmares. Clonidine ("Catapres") can be helpful with startle, hyperarousal, and general autonomic hyperexcitability. as well as mood or aggression. Topiramate ("Topamax") Valproic acid ("Depakene") and has shown reduction of symptoms of irritability, aggression, and impulsiveness, and in reducing flashbacks. Nefazodone ("Serzone") can be effective with sleep disturbance symptoms, and with secondary depression, anxiety, and sexual dysfunction symptoms. hyperarousal, and sleep disturbance.
Glucocorticoids. Additionally, post-stress high dose corticosterone administration was recently found to reduce 'PTSD-like' behaviors in a rat model of PTSD. In this study, corticosterone impaired memory performance, suggesting that it may reduce risk for PTSD by interfering with consolidation of traumatic memories. The neurodegenerative effects of the glucocorticoids, however, may prove this treatment counterproductive.
Heterocyclic / Tricyclic anti-depressants anti-depressants. Amitriptyline ("Elavil") has shown benefit for positive distress symptoms, and for avoidance, and Imipramine ("Tofranil") has shown benefit for intrusive symptoms. and Israel.
Alpha-adrenergic antagonists. Anecdotal report of success in using clonidine ("Catapres") to reduce traumatic stress symptoms suggests that it may have benefit in preventing PTSD.
Beta blockers. Propranolol ("Inderal"), similarly to clonidine, may be useful if there are significant symptoms of "over-arousal". These may inhibit the formation of traumatic memories by blocking adrenaline's effects on the amygdala.
Glucocorticoids. There is some evidence suggesting that administering glucocorticoids immediately after a traumatic experience may help prevent PTSD. Several studies have shown that individuals who receive high doses of hydrocortisone for treatment of septic shock, or following surgery, have a lower incidence and fewer symptoms of PTSD.
Opiates. In a retrospective analysis of combat injury field data for US troops in Iraq, it was found that those who received morphine in the early stages of their treatment had a significantly lower rate of subsequent PTSD, when compared with those who did not receive morphine at that time.
Some medications can also help with symptoms which may occur secondary to PTSD.
Benzodiazepines are risky in several ways. They can be especially addictive when PTSD is present, and this is especially true with the fast-acting ones. Dis-inhibition upon initiation of treatment is another risk with this medication class. Finally, termination of the drug can be especially difficult.]] There is debate over the rates of PTSD found in populations, but despite changes in diagnosis and the criteria used to define PTSD between 1997 and 2007, epidemiological rates have not changed significantly.
{| class="wikitable" border="1" |+ Age-standardized Disability-adjusted life year (DALY) rates for PTSD, per 100,000 inhabitants, in 25 most populous countries, The National Vietnam Veterans' Readjustment Study (NVVRS) found 15.2% of male and 8.5% of female Vietnam Vets to suffer from current PTSD at the time of the study. Life-Time prevalence of PTSD was 30.9% for males and 26.9% for females. In a reanalysis of the NVVRS data, along with analysis of the data from the Matsunaga Vietnam Veterans Project, Schnurr, Lunney, Sengupta, and Waelde found that, contrary to the initial analysis of the NVVRS data, a large majority of Vietnam veterans suffered from PTSD symptoms (but not the disorder itself). Four out of five reported recent symptoms when interviewed 20–25 years after Vietnam. and wild elephants suffering from posttraumatic stress reactions, the latter from seeing members of their herd shot by hunters. Service dogs used overseas in the military have been said to develop posttraumatic stress after witnessing war.
According to Stéphane Audoin-Rouzeau and Annette Becker, "One-tenth of mobilized American men were hospitalized for mental disturbances between 1942 and 1945, and after thirty-five days of uninterrupted combat, 98% of them manifested psychiatric disturbances in varying degrees."
Although PTSD-like symptoms have also been recognized in combat veterans of many military conflicts since, the modern understanding of PTSD dates from the 1970s, largely as a result of the problems that were still being experienced by US military veterans of the war in Vietnam.
Early in 1978, the term was used in a working group finding presented to the Committee of Reactive Disorders. The term was formally recognized in 1980. (In the authoritative DSM-IV, the spelling "posttraumatic stress disorder" is used. Elsewhere, "posttraumatic" is often rendered as two words — "post-traumatic stress disorder" or "post traumatic stress disorder" — especially in less formal writing on the subject.)
Category:Abnormal psychology Category:Alcohol abuse Category:Anxiety disorders Category:Counseling Category:Homelessness Category:Military medicine Category:Military personnel Category:Military psychiatry Category:Military sociology Category:Military veterans' affairs Category:Mood disorders Category:Neurotic, stress-related and somatoform disorders Category:Rape Category:Stress Category:Traumatology
This text is licensed under the Creative Commons CC-BY-SA License. This text was originally published on Wikipedia and was developed by the Wikipedia community.
