
- Order:
- Duration: 3:39
- Published: 11 Sep 2007
- Uploaded: 11 May 2011
- Author: NationalGeographic



































































Obesity increases the likelihood of various diseases, particularly heart disease, type 2 diabetes, breathing difficulties during sleep, certain types of cancer, and osteoarthritis.
Dieting and physical exercise are the mainstays of treatment for obesity. Moreover, it is important to improve diet quality by reducing the consumption of energy-dense foods such as those high in fat and sugars, and by increasing the intake of dietary fiber. To supplement this, or in case of failure, anti-obesity drugs may be taken to reduce appetite or inhibit fat absorption. In severe cases, surgery is performed or an intragastric balloon is placed to reduce stomach volume and/or bowel length, leading to earlier satiation and reduced ability to absorb nutrients from food.
Obesity is a leading preventable cause of death worldwide, with increasing prevalence in adults and children, and authorities view it as one of the most serious public health problems of the 21st century. Obesity is stigmatized in much of the modern world (particularly in the Western world), though it was widely perceived as a symbol of wealth and fertility at other times in history, and still is in some parts of the world. BMI is closely related to both percentage body fat and total body fat.
In children, a healthy weight varies with age and sex. Obesity in children and adolescents is defined not as an absolute number, but in relation to a historical normal group, such that obesity is a BMI greater than the 95th percentile. The reference data on which these percentiles are based are from 1963 to 1994, and thus have not been affected by the recent increases in weight.
BMI is calculated by dividing the subject's mass by the square of his or her height, typically expressed either in metric or US "customary" units:
:Metric:
:US customary and imperial:
where is the subject's weight in pounds and is the subject's height in inches.
The most commonly used definitions, established by the World Health Organization (WHO) in 1997 and published in 2000, provide the values listed in the table at right.
As Asian populations develop negative health consequences at a lower BMI than Caucasians, some nations have redefined obesity; the Japanese have defined obesity as any BMI greater than 25 while China uses a BMI of greater than 28.
Obesity is one of the leading preventable causes of death worldwide. Large-scale American and European studies have found that mortality risk is lowest at a BMI of 20–25 kg/m2 A BMI above 32 has been associated with a doubled mortality rate among women over a 16-year period. In the United States obesity is estimated to cause an excess 111,909 to 365,000 deaths per year, On average, obesity reduces life expectancy by six to seven years: a BMI of 30–35 reduces life expectancy by two to four years,
Complications are either directly caused by obesity or indirectly related through mechanisms sharing a common cause such as a poor diet or a sedentary lifestyle. The strength of the link between obesity and specific conditions varies. One of the strongest is the link with type 2 diabetes. Excess body fat underlies 64% of cases of diabetes in men and 77% of cases in women.
Health consequences fall into two broad categories: those attributable to the effects of increased fat mass (such as osteoarthritis, obstructive sleep apnea, social stigmatization) and those due to the increased number of fat cells (diabetes, cancer, cardiovascular disease, non-alcoholic fatty liver disease). Increases in body fat alter the body's response to insulin, potentially leading to insulin resistance. Increased fat also creates a proinflammatory state, and a prothrombotic state.
In people with heart failure, those with a BMI between 30.0–34.9 had lower mortality than those with a normal weight. This has been attributed to the fact that people often lose weight as they become progressively more ill. Similar findings have been made in other types of heart disease. People with class I obesity and heart disease do not have greater rates of further heart problems than people of normal weight who also have heart disease. In people with greater degrees of obesity, however, risk of further events is increased. Even after cardiac bypass surgery, no increase in mortality is seen in the overweight and obese. One study found that the improved survival could be explained by the more aggressive treatment obese people receive after a cardiac event. Another found that if one takes into account chronic obstructive pulmonary disease (COPD) in those with PAD the benefit of obesity no longer exists. In contrast, increasing rates of obesity at a societal level are felt to be due to an easily accessible and palatable diet, increased reliance on cars, and mechanized manufacturing.
A 2006 review identified ten other possible contributors to the recent increase of obesity: (1) insufficient sleep, (2) endocrine disruptors (environmental pollutants that interfere with lipid metabolism), (3) decreased variability in ambient temperature, (4) decreased rates of smoking, because smoking suppresses appetite, (5) increased use of medications that can cause weight gain (e.g., atypical antipsychotics), (6) proportional increases in ethnic and age groups that tend to be heavier, (7) pregnancy at a later age (which may cause susceptibility to obesity in children), (8) epigenetic risk factors passed on generationally, (9) natural selection for higher BMI, and (10) assortative mating leading to increased concentration of obesity risk factors (this would not necessarily increase the number of obese people, but would increase the average population weight). While there is substantial evidence supporting the influence of these mechanisms on the increased prevalence of obesity, the evidence is still inconclusive, and the authors state that these are probably less influential than the ones discussed in the previous paragraph.
Before the 20th century, obesity was rare; The rate of obesity also increases with age at least up to 50 or 60 years old and severe obesity in the United States, Australia, and Canada is increasing faster than the overall rate of obesity.
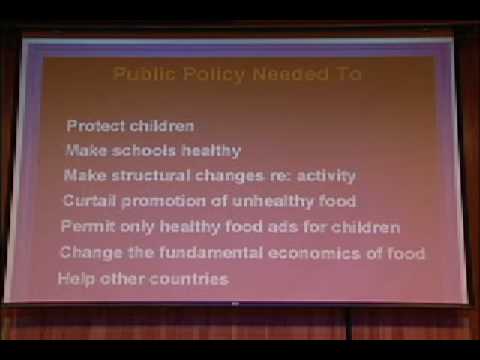
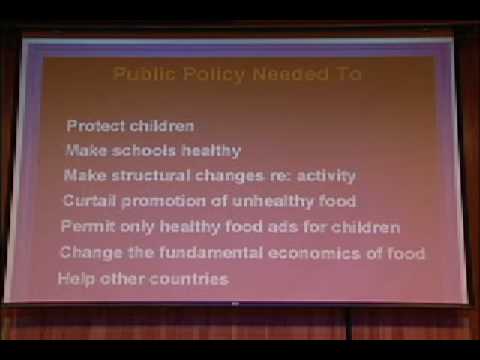
Once considered a problem only of high-income countries, obesity rates are rising worldwide and affecting both the developed and developing world. These increases have been felt most dramatically in urban settings. Obesity is a public health and policy problem because of its prevalence, costs, and health effects. Public health efforts seek to understand and correct the environmental factors responsible for the increasing prevalence of obesity in the population. Solutions look at changing the factors that cause excess calorie consumption and inhibit physical activity. Efforts include federally reimbursed meal programs in schools, limiting direct junk food marketing to children, and decreasing access to sugar-sweetened beverages in schools. When constructing urban environments, efforts have been made to increase access to parks and to develop pedestrian routes.
Many countries and groups have published reports pertaining to obesity. In 1998 the first US Federal guidelines were published, titled "Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report". In 2006 the Canadian Obesity Network published the "Canadian Clinical Practice Guidelines (CPG) on the Management and Prevention of Obesity in Adults and Children". This is a comprehensive evidence-based guideline to address the management and prevention of overweight and obesity in adults and children.
In 2004, the United Kingdom Royal College of Physicians, the Faculty of Public Health and the Royal College of Paediatrics and Child Health released the report "Storing up Problems", which highlighted the growing problem of obesity in the UK. The same year, the House of Commons Health Select Committee published its "most comprehensive inquiry [...] ever undertaken" into the impact of obesity on health and society in the UK and possible approaches to the problem. In 2006, the National Institute for Health and Clinical Excellence (NICE) issued a guideline on the diagnosis and management of obesity, as well as policy implications for non-healthcare organizations such as local councils.
A 2007 report produced by Sir Derek Wanless for the King's Fund warned that unless further action was taken, obesity had the capacity to cripple the National Health Service financially. In the United States organizations such as the Bill Clinton Foundation's Alliance for a Healthier Generation and Action for Healthy Kids are working to combat childhood obesity. Additionally, the Centers for Disease Control and Prevention co-hosted the first-ever Weight of the Nation Conference in 2009 with the goal of focusing national attention on the obesity epidemic.
Comprehensive approaches are being looked at to address the rising rates of obesity. The Obesity Policy Action (OPA) framework divides measure into 'upstream' policies, 'midstream' policies, 'downstream' policies. 'Upstream' policies look at changing society, 'midstream' policies try to alter individuals' behavior to prevent obesity, and 'downstream' policies try to treat currently afflicted people.
The estimate range for annual expenditures on diet products is $40 billion to $100 billion in the US alone. In 1998, the medical costs attributable to obesity in the US were $78.5 billion or 9.1% of all medical expenditures, while the cost of obesity in Canada was estimated at CA$2 billion in 1997 (2.4% of total health costs).
Obesity can lead to social stigmatization and disadvantages in employment. A study examining Duke University employees found that people with a BMI over 40 filed twice as many workers' compensation claims as those whose BMI was 18.5–24.9. They also had more than 12 times as many lost work days. The most common injuries in this group were due to falls and lifting, thus affecting the lower extremities, wrists or hands, and backs. The US state of Alabama Employees' Insurance Board approved a controversial plan to charge obese workers $25 per month if they do not take measures to reduce their weight and improve their health. These measures started in January 2010 and apply to those with a BMI of greater than 35 kg/m2 who fail to make improvements in their health after one year.
Some research shows that obese people are less likely to be hired for a job and are less likely to be promoted.
Specific industries, such as the airline and food industries, have special concerns. Due to rising rates of obesity, airlines face higher fuel costs and pressures to increase seating width. In 2000, the extra weight of obese passengers cost airlines US$275 million. Costs for restaurants are increased by litigation accusing them of causing obesity. In 2005 the US Congress discussed legislation to prevent civil law suits against the food industry in relation to obesity; however, it did not become law. The Oxford English Dictionary documents its first usage in 1611 by Randle Cotgrave.
With the onset of the industrial revolution it was realized that the military and economic might of nations were dependent on both the body size and strength of their soldiers and workers. During this time period insurance companies realized the connection between weight and life expectancy and increased premiums for the obese.
created 24,000–22,000 BC]] Public perceptions in Western society regarding healthy body weight differ from those regarding the weight that is considered ideal – and both have changed since the beginning of the 20th century. The weight that is viewed as an ideal has become lower since the 1920s. This is illustrated by the fact that the average height of Miss America pageant winners increased by 2% from 1922 to 1999, while their average weight decreased by 12%. On the other hand, people's views concerning healthy weight have changed in the opposite direction. In Britain the weight at which people considered themselves to be overweight was significantly higher in 2007 than in 1999. These changes are believed to be due to increasing rates of adiposity leading to increased acceptance of extra body fat as being normal. Rubens (1577–1640) regularly depicted full-bodied women in his pictures, from which derives the term Rubenesque. These women, however, still maintained the "hourglass" shape with its relationship to fertility. During the 19th century, views on obesity changed in the Western world. After centuries of obesity being synonymous with wealth and social status, slimness began to be seen as the desirable standard. However, some in the movement are also attempting to challenge the established relationship between obesity and negative health outcomes.
A number of organizations exist that promote the acceptance of obesity. They have increased in prominence in the latter half of the 20th century. The US-based National Association to Advance Fat Acceptance (NAAFA) was formed in 1969 and describes itself as a civil rights organization dedicated to ending size discrimination.
The International Size Acceptance Association (ISAA) is a non-governmental organization (NGO) which was founded in 1997. It has more of a global orientation and describes its mission as promoting size acceptance and helping to end weight-based discrimination. These groups often argue for the recognition of obesity as a disability under the US Americans With Disabilities Act (ADA). The American legal system, however, has decided that the potential public health costs exceed the benefits of extending this anti-discrimination law to cover obesity. Similarly, The Obesity Epidemic by Michael Gard argues that obesity is a moral and ideological construct, rather than a health problem. Other groups are also trying to challenge obesity's connection to poor health. The Center for Consumer Freedom, an organization partly supported by the restaurant and food industry, has run ads saying that obesity is not an epidemic but "hype".
People are known to select potential partners based on a similar body mass. The rising rates of obesity have therefore provided greater opportunities for overweight people to find partners. Certain subcultures also label themselves as particularly attracted to the obese. Chubby culture and fat admirers are examples.
Category:Metabolic disorders Category:Nutrition Category:Bariatrics Category:Body shape
This text is licensed under the Creative Commons CC-BY-SA License. This text was originally published on Wikipedia and was developed by the Wikipedia community.
| Name | Richard Carmona |
|---|---|
| Caption | Vice Admiral Richard Carmona, USPHSSurgeon General of the United States |
| Order | 17th |
| Title | Surgeon General of the United States |
| President | George W. Bush |
| Term start | August 5, 2002 |
| Term end | July 31, 2006 |
| Predecessor | David Satcher |
| Successor | Regina Benjamin |
| Birth date | November 22, 1949 |
| Birth place | New York, New York, USA |
| Party | Republican |
Richard Henry Carmona (born 22 November 1949) is an American physician and public health administrator. He was a vice admiral in the Public Health Service Commissioned Corps and served as the seventeenth Surgeon General of the United States. Appointed by President George W. Bush in 2002, Carmona left office at the end of July 2006 upon the expiration of his term. After leaving office, Carmona was highly critical of the Bush Administration for interfering with and suppressing scientific findings which conflicted with the Administration's ideological agenda.
In August 2006, Carmona returned home to Tucson, Arizona. He is now vice chairman of the Canyon Ranch resort and spa company, president of the non-profit Canyon Ranch Institute, and a professor at the Mel and Enid Zuckerman College of Public Health at the University of Arizona.
After leaving active duty, Carmona attended the Bronx Community College of the City University of New York, where he earned his associate of arts degree in nursing. In 1977, he graduated from the University of California, San Francisco (UCSF), with a bachelor of science degree; in 1979, he received his medical degree from UCSF, where he was awarded the prestigious gold headed cane as the top graduate.
In 1998, he earned a Master's degree in Public Health (M.P.H.) from the University of Arizona.
Before being named Surgeon General, Carmona was the chairman of the State of Arizona Southern Regional Emergency Medical System, a professor of surgery, public health and family and community medicine at the University of Arizona, and the Pima County Sheriff's Department surgeon and deputy sheriff.
Carmona has held positions of responsibility as chief medical officer, hospital chief executive officer, public health officer, and finally chief executive officer of the Pima County health care system. He has also served as a medical director of police and fire departments and is a peace officer with expertise in special operations and emergency preparedness, including weapons of mass destruction. On June 16, 2010, Ross University School of Medicine named Carmona to its Board of Trustees.
Carmona also testified that the Bush Administration had attempted for years to "water down" his report on the dangers of secondhand smoke and pressured him not to testify in the tobacco industry's racketeering trial: "Anything that doesn't fit into the political appointees' ideological, theological or political agenda is ignored, marginalized or simply buried." According to Carmona, he was even ordered not to attend the Special Olympics because the event was sponsored by the Kennedy family, and was told to mention President Bush three times on every page of his speeches. The Washington Post subsequently identified William R. Steiger as the Bush Administration official who had blocked release of Carmona's report on global health because it conflicted with the Administration's political priorities.
Reuters reported that Carmona's predecessors as Surgeon General had acknowledged the high level of political interference he experienced, saying: "We have never seen it as partisan, as malicious, as vindictive, as mean-spirited as it is today, and you clearly have worse than anyone's had."
Category:American military personnel of the Vietnam War Category:American nurses Category:American surgeons Category:City University of New York alumni Category:DeWitt Clinton High School alumni Category:George W. Bush administration controversies Category:Paramedics Category:People from Manhattan Category:Puerto Rican Army personnel Category:Recipients of the Bronze Star Medal Category:Recipients of the Purple Heart medal Category:Surgeons General of the United States Category:University of Arizona alumni Category:University of Arizona faculty Category:University of California, San Francisco alumni Category:1949 births Category:Living people Category:People from Pima County, Arizona
This text is licensed under the Creative Commons CC-BY-SA License. This text was originally published on Wikipedia and was developed by the Wikipedia community.