- Order:
- Duration: 20:12
- Published: 2008-03-13
- Uploaded: 2011-02-02
- Author: TEDtalksDirector
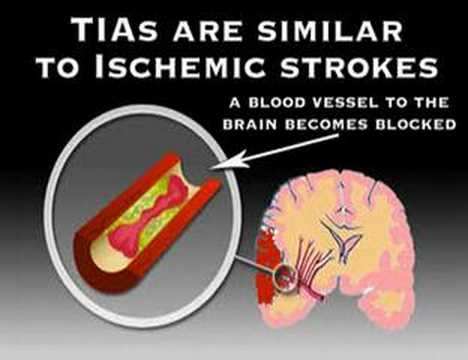
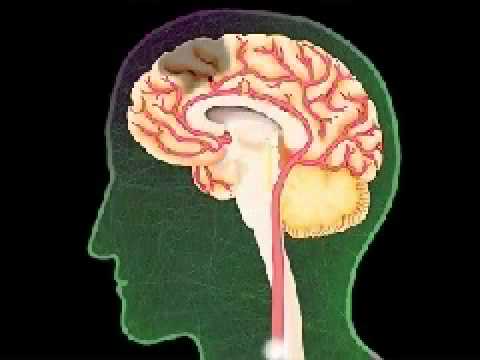
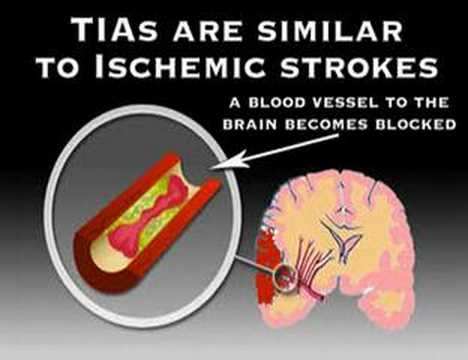
A stroke is a medical emergency and can cause permanent neurological damage, complications, and even death. It is the leading cause of adult disability in the United States and Europe and it is the number two cause of death worldwide. Risk factors for stroke include advanced age, hypertension (high blood pressure), previous stroke or transient ischemic attack (TIA), diabetes, high cholesterol, cigarette smoking and atrial fibrillation. High blood pressure is the most important modifiable risk factor of stroke. is a "neurological deficit of cerebrovascular cause that persists beyond 24 hours or is interrupted by death within 24 hours". This definition was supposed to reflect the reversibility of tissue damage and was devised for the purpose, with the time frame of 24 hours being chosen arbitrarily. The 24-hour limit divides stroke from transient ischemic attack, which is a related syndrome of stroke symptoms that resolve completely within 24 hours.
Stroke without an obvious explanation is termed "cryptogenic" (of unknown origin); this constitutes 30-40% of all ischemic strokes.
There are various classification systems for acute ischemic stroke. The Oxford Community Stroke Project classification (OCSP, also known as the Bamford or Oxford classification) relies primarily on the initial symptoms; based on the extent of the symptoms, the stroke episode is classified as total anterior circulation infarct (TACI), partial anterior circulation infarct (PACI), lacunar infarct (LACI) or posterior circulation infarct (POCI). These four entities predict the extent of the stroke, the area of the brain affected, the underlying cause, and the prognosis. The TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification is based on clinical symptoms as well as results of further investigations; on this basis, a stroke is classified as being due to (1) thrombosis or embolism due to atherosclerosis of a large artery, (2) embolism of cardiac origin, (3) occlusion of a small blood vessel, (4) other determined cause, (5) undetermined cause (two possible causes, no cause identified, or incomplete investigation).
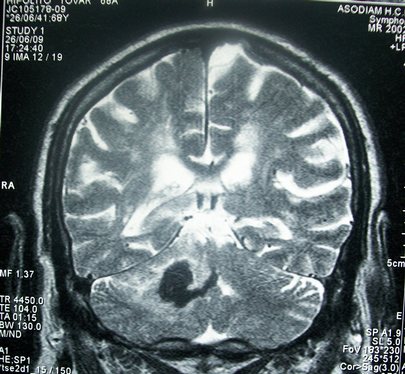
Intracranial hemorrhage is the accumulation of blood anywhere within the skull vault. A distinction is made between intra-axial hemorrhage (blood inside the brain) and extra-axial hemorrhage (blood inside the skull but outside the brain). Intra-axial hemorrhage is due to intraparenchymal hemorrhage or intraventricular hemorrhage (blood in the ventricular system). The main types of extra-axial hemorrhage are epidural hematoma (bleeding between the dura mater and the skull), subdural hematoma (in the subdural space) and subarachnoid hemorrhage (between the arachnoid mater and pia mater). Most of the hemorrhagic stroke syndromes have specific symptoms (e.g. headache, previous head injury).
Proposed systems include FAST (face, arm, speech, and time), as advocated by the Department of Health (United Kingdom) and The Stroke Association, the American Stroke Association (www.strokeassociation.org) , National Stroke Association (US www.stroke.org), the Los Angeles Prehospital Stroke Screen (LAPSS) and the Cincinnati Prehospital Stroke Scale (CPSS). Use of these scales is recommended by professional guidelines.
For people referred to the emergency room, early recognition of stroke is deemed important as this can expedite diagnostic tests and treatments. A scoring system called ROSIER (recognition of stroke in the emergency room) is recommended for this purpose; it is based on features from the medical history and physical examination.
In most cases, the symptoms affect only one side of the body (unilateral). Depending on the part of the brain affected, the defect in the brain is usually on the opposite side of the body. However, since these pathways also travel in the spinal cord and any lesion there can also produce these symptoms, the presence of any one of these symptoms does not necessarily indicate a stroke.
In addition to the above CNS pathways, the brainstem also consists of the 12 cranial nerves. A stroke affecting the brain stem therefore can produce symptoms relating to deficits in these cranial nerves:
If the cerebral cortex is involved, the CNS pathways can again be affected, but also can produce the following symptoms:
If the cerebellum is involved, the patient may have the following:
If symptoms are maximal at onset, the cause is more likely to be a subarachnoid hemorrhage or an embolic stroke.
Sickle cell anemia, which can cause blood cells to clump up and block blood vessels, can also lead to stroke. A stroke is the second leading killer of people under 20 who suffer from sickle-cell anemia.
;Systemic hypoperfusion Systemic hypoperfusion is the reduction of blood flow to all parts of the body. It is most commonly due to cardiac pump failure from cardiac arrest or arrhythmias, or from reduced cardiac output as a result of myocardial infarction, pulmonary embolism, pericardial effusion, or bleeding. Hypoxemia (low blood oxygen content) may precipitate the hypoperfusion. Because the reduction in blood flow is global, all parts of the brain may be affected, especially "watershed" areas - border zone regions supplied by the major cerebral arteries. A watershed stroke refers to the condition when blood supply to these areas is compromised. Blood flow to these areas does not necessarily stop, but instead it may lessen to the point where brain damage can occur. This phenomenon is also referred to as "last meadow" to point to the fact that in irrigation the last meadow receives the least amount of water.
;Venous thrombosis Cerebral venous sinus thrombosis leads to stroke due to locally increased venous pressure, which exceeds the pressure generated by the arteries. Infarcts are more likely to undergo hemorrhagic transformation (leaking of blood into the damaged area) than other types of ischemic stroke. Brain tissue ceases to function if deprived of oxygen for more than 60 to 90 seconds and after approximately three hours, will suffer irreversible injury possibly leading to death of the tissue, i.e., infarction. (This is why TPA's (e.g. Streptokinase, Altapase) are given only until three hours since the onset of the stroke.) Atherosclerosis may disrupt the blood supply by narrowing the lumen of blood vessels leading to a reduction of blood flow, by causing the formation of blood clots within the vessel, or by releasing showers of small emboli through the disintegration of atherosclerotic plaques. Embolic infarction occurs when emboli formed elsewhere in the circulatory system, typically in the heart as a consequence of atrial fibrillation, or in the carotid arteries, break off, enter the cerebral circulation, then lodge in and occlude brain blood vessels. Since blood vessels in the brain are now occluded, the brain becomes low in energy, and thus it resorts into using anaerobic respiration within the region of brain tissue affected by ischemia. Unfortunately, this kind of respiration produces less adenosine triphosphate (ATP) but releases a by-product called lactic acid. Lactic acid is an irritant which could potentially destroy cells since it is an acid and disrupts the normal acid-base balance in the brain. The ischemia area is referred to as the "ischemic penumbra".
Then, as oxygen or glucose becomes depleted in ischemic brain tissue, the production of high energy phosphate compounds such as adenosine triphosphate (ATP) fails, leading to failure of energy-dependent processes (such as ion pumping) necessary for tissue cell survival. This sets off a series of interrelated events that result in cellular injury and death. A major cause of neuronal injury is release of the excitatory neurotransmitter glutamate. The concentration of glutamate outside the cells of the nervous system is normally kept low by so-called uptake carriers, which are powered by the concentration gradients of ions (mainly Na+) across the cell membrane. However, stroke cuts off the supply of oxygen and glucose which powers the ion pumps maintaining these gradients. As a result the transmembrane ion gradients run down, and glutamate transporters reverse their direction, releasing glutamate into the extracellular space. Glutamate acts on receptors in nerve cells (especially NMDA receptors), producing an influx of calcium which activates enzymes that digest the cells' proteins, lipids and nuclear material. Calcium influx can also lead to the failure of mitochondria, which can lead further toward energy depletion and may trigger cell death due to apoptosis.
Ischemia also induces production of oxygen free radicals and other reactive oxygen species. These react with and damage a number of cellular and extracellular elements. Damage to the blood vessel lining or endothelium is particularly important. In fact, many antioxidant neuroprotectants such as uric acid and NXY-059 work at the level of the endothelium and not in the brain per se. Free radicals also directly initiate elements of the apoptosis cascade by means of redox signaling. This agent appears to work at the level of the blood vessel lining or endothelium. Unfortunately, after producing favorable results in one large-scale clinical trial, a second trial failed to show favorable results.
For diagnosing hemorrhagic stroke in the emergency setting:
For detecting chronic hemorrhages, MRI scan is more sensitive.
For the assessment of stable stroke, nuclear medicine scans SPECT and PET/CT may be helpful. SPECT documents cerebral blood flow and PET with FDG isotope the metabolic activity of the neurons.
No high quality studies have shown the effectiveness of interventions aimed at weight reduction, promotion of regular exercise, reducing alcohol consumption or smoking cessation. Nonetheless, given the large body of circumstantial evidence, best medical management for stroke includes advice on diet, exercise, smoking and alcohol use. Medication or drug therapy is the most common method of stroke prevention; carotid endarterectomy can be a useful surgical method of preventing stroke.
In primary prevention however, antiplatelet drugs did not reduce the risk of ischemic stroke while increasing the risk of major bleeding. Further studies are needed to investigate a possible protective effect of aspirin against ischemic stroke in women.
Screening for carotid artery narrowing has not been shown to be a useful screening test in the general population. Studies of surgical intervention for carotid artery stenosis without symptoms have shown only a small decrease in the risk of stroke. To be beneficial, the complication rate of the surgery should be kept below 4%. Even then, for 100 surgeries, 5 patients will benefit by avoiding stroke, 3 will develop stroke despite surgery, 3 will develop stroke or die due to the surgery itself, and 89 will remain stroke-free but would also have done so without intervention.
With regards to lowering homocysteine, a meta-analysis of previous trials has concluded that lowering homocysteine with folic acid and other supplements may reduce stroke risk. However, the two largest randomized controlled trials included in the meta-analysis had conflicting results. One reported positive results; whereas the other was negative.
The European Society of Cardiology and the European Association for Cardiovascular Prevention and Rehabilitation have developed an interactive tool for prediction and managing the risk of heart attack and stroke in Europe. HeartScore is aimed at supporting clinicians in optimising individual cardiovascular risk reduction. The Heartscore Programme is available in 12 languages and offers web based or PC version.
Other medical therapies are aimed at minimizing clot enlargement or preventing new clots from forming. To this end, treatment with medications such as aspirin, clopidogrel and dipyridamole may be given to prevent platelets from aggregating. which showed that tPA improves the chances for a good neurological outcome. When administered within the first three hours, 39% of all patients who were treated with tPA had a good outcome at three months, only 26% of placebo controlled patients had a good functional outcome. A recent study using alteplase for thrombolysis in ischemic stroke suggests clinical benefit with administration 3 to 4.5 hours after stroke onset. However, in the NINDS trial 6.4% of patients with large strokes developed substantial brain hemorrhage as a complication from being given tPA. A recent study found the mortality to be higher among patients receiving tPA versus those who did not. Additionally, it is the position of the American Academy of Emergency Medicine that objective evidence regarding the efficacy, safety, and applicability of tPA for acute ischemic stroke is insufficient to warrant its classification as standard of care.
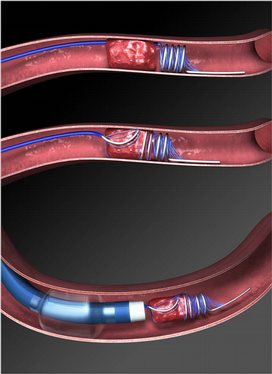
Intra-arterial fibrinolysis, where a catherter is passed up an artery into the brain and the medication is injected at the site of thrombosis, has been found to improve outcomes in people with acute ischemic stroke.
Another intervention for acute ischemic stroke is removal of the offending thrombus directly. This is accomplished by inserting a catheter into the femoral artery, directing it into the cerebral circulation, and deploying a corkscrew-like device to ensnare the clot, which is then withdrawn from the body. Mechanical embolectomy devices have been demonstrated effective at restoring blood flow in patients who were unable to receive thrombolytic drugs or for whom the drugs were ineffective, though no differences have been found between newer and older versions of the devices. The devices have only been tested on patients treated with mechanical clot embolectomy within eight hours of the onset of symptoms.
Most of the data concerning therapeutic hypothermia’s effectiveness in treating ischemic stroke is limited to animal studies. These studies have focused primarily on ischemic as opposed to hemorrhagic stroke, as hypothermia has been associated with a lower clotting threshold. In these animal studies investigating the effect of temperature decline following ischemic stroke, hypothermia has been shown to be an effective all-purpose neuroprotectant. This promising data has led to the initiation of a variety of human studies. At the time of this article’s publishing, this research has yet to return results. However, in terms of feasibility, the use of hypothermia to control intracranial pressure (ICP) after an ischemic stroke was found to be both safe and practical. The device used in this study was called the Arctic Sun.
If studies show carotid stenosis, and the patient has residual function in the affected side, carotid endarterectomy (surgical removal of the stenosis) may decrease the risk of recurrence if performed rapidly after stroke.
A rehabilitation team is usually multidisciplinary as it involves staff with different skills working together to help the patient. These include nursing staff, physiotherapy, occupational therapy, speech and language therapy, and usually a physician trained in rehabilitation medicine. Some teams may also include psychologists, social workers, and pharmacists since at least one third of the patients manifest post stroke depression. Validated instruments such as the Barthel scale may be used to assess the likelihood of a stroke patient being able to manage at home with or without support subsequent to discharge from hospital.
Good nursing care is fundamental in maintaining skin care, feeding, hydration, positioning, and monitoring vital signs such as temperature, pulse, and blood pressure. Stroke rehabilitation begins almost immediately.
For most stroke patients, physical therapy (PT) and occupational therapy (OT), speech-language pathology (SLP) are the cornerstones of the rehabilitation process. Often, assistive technology such as a wheelchair, walkers, canes, and orthosis may be beneficial. PT and OT have overlapping areas of working but their main attention fields are; PT involves re-learning functions as transferring, walking and other gross motor functions. OT focusses on exercises and training to help relearn everyday activities known as the Activities of daily living (ADLs) such as eating, drinking, dressing, bathing, cooking, reading and writing, and toileting. Speech and language therapy is appropriate for patients with the speech production disorders: dysarthria and apraxia of speech, aphasia, cognitive-communication impairments and/or dysphagia (problems with swallowing).
Patients may have particular problems, such as complete or partial inability to swallow, which can cause swallowed material to pass into the lungs and cause aspiration pneumonia. The condition may improve with time, but in the interim, a nasogastric tube may be inserted, enabling liquid food to be given directly into the stomach. If swallowing is still deemed unsafe, then a percutaneous endoscopic gastrostomy (PEG) tube is passed and this can remain indefinitely.
Stroke rehabilitation should be started as quickly as possible and can last anywhere from a few days to over a year. Most return of function is seen in the first few months, and then improvement falls off with the "window" considered officially by U.S. state rehabilitation units and others to be closed after six months, with little chance of further improvement. However, patients have been known to continue to improve for years, regaining and strengthening abilities like writing, walking, running, and talking. Daily rehabilitation exercises should continue to be part of the stroke patient's routine. Complete recovery is unusual but not impossible and most patients will improve to some extent : proper diet and exercise are known to help the brain to recover.
Disability affects 75% of stroke survivors enough to decrease their employability. Stroke can affect patients physically, mentally, emotionally, or a combination of the three. The results of stroke vary widely depending on size and location of the lesion. Dysfunctions correspond to areas in the brain that have been damaged.
Some of the physical disabilities that can result from stroke include muscle weakness, numbness, pressure sores, pneumonia, incontinence, apraxia (inability to perform learned movements), difficulties carrying out daily activities, appetite loss, speech loss, vision loss, and pain. If the stroke is severe enough, or in a certain location such as parts of the brainstem, coma or death can result.
Emotional problems resulting from stroke can result from direct damage to emotional centers in the brain or from frustration and difficulty adapting to new limitations. Post-stroke emotional difficulties include anxiety, panic attacks, flat affect (failure to express emotions), mania, apathy, and psychosis.
30 to 50% of stroke survivors suffer post stroke depression, which is characterized by lethargy, irritability, sleep disturbances, lowered self esteem, and withdrawal. Depression can reduce motivation and worsen outcome, but can be treated with antidepressants.
Emotional lability, another consequence of stroke, causes the patient to switch quickly between emotional highs and lows and to express emotions inappropriately, for instance with an excess of laughing or crying with little or no provocation. While these expressions of emotion usually correspond to the patient's actual emotions, a more severe form of emotional lability causes patients to laugh and cry pathologically, without regard to context or emotion. Emotional lability occurs in about 20% of stroke patients.
Cognitive deficits resulting from stroke include perceptual disorders, speech problems, dementia, and problems with attention and memory. A stroke sufferer may be unaware of his or her own disabilities, a condition called anosognosia. In a condition called hemispatial neglect, a patient is unable to attend to anything on the side of space opposite to the damaged hemisphere.
Up to 10% of all stroke patients develop seizures, most commonly in the week subsequent to the event; the severity of the stroke increases the likelihood of a seizure.
The incidence of stroke increases exponentially from 30 years of age, and etiology varies by age. Advanced age is one of the most significant stroke risk factors. 95% of strokes occur in people age 45 and older, and two-thirds of strokes occur in those over the age of 65. A person's risk of dying if he or she does have a stroke also increases with age. However, stroke can occur at any age, including in childhood.
Family members may have a genetic tendency for stroke or share a lifestyle that contributes to stroke. Higher levels of Von Willebrand factor are more common amongst people who have had ischemic stroke for the first time. The results of this study found that the only significant genetic factor was the person's blood type. Having had a stroke in the past greatly increases one's risk of future strokes.
Men are 25% more likely to suffer strokes than women, Hippocrates (460 to 370 BC) was first to describe the phenomenon of sudden paralysis that is often associated with ischemia. Apoplexy, from the Greek word meaning "struck down with violence,” first appeared in Hippocratic writings to describe this phenomenon.
The word stroke was used as a synonym for apoplectic seizure as early as 1599, and is a fairly literal translation of the Greek term.
In 1658, in his Apoplexia, Johann Jacob Wepfer (1620–1695) identified the cause of hemorrhagic stroke when he suggested that people who had died of apoplexy had bleeding in their brains.
Category:Aging-associated diseases Category:Cerebrovascular diseases
This text is licensed under the Creative Commons CC-BY-SA License. This text was originally published on Wikipedia and was developed by the Wikipedia community.